Diabetes mellitus is a group of metabolic diseases characterized by chronic hyperglycemia resulting from defects in insulin secretion, insulin action, or both. Metabolic abnormalities in carbohydrates, lipids, and proteins result from the importance of insulin as an anabolic hormone. Low levels of insulin to achieve adequate response and/or insulin resistance of target tissues, mainly skeletal muscles, adipose tissue, and to a lesser extent, liver, at the level of insulin receptors, signal transduction system, and/or effector enzymes or genes are responsible for these metabolic abnormalities. The severity of symptoms is due to the type and duration of diabetes. Some of the diabetes patients are asymptomatic especially those with type 2 diabetes during the early years of the disease, others with marked hyperglycemia and especially in children with absolute insulin deficiency may suffer from polyuria, polydipsia, polyphagia, weight loss, and blurred vision. Uncontrolled diabetes may lead to stupor, coma and if not treated death, due to ketoacidosis or rare from nonketotic hyperosmolar syndrome[rx–rx].
Types of Diabetes Mellitus
Type 1 Diabetes Mellitus (T1DM)
- Type 1 diabetes mellitus (T1DM) is an autoimmune disease that leads to the destruction of the insulin-producing pancreatic beta cells. Insulin is an essential anabolic hormone that exerts multiple effects on glucose, lipid, protein and mineral metabolism, as well as growth. Importantly, insulin allows glucose to enter muscle and adipose cells, stimulates the liver to store glucose as glycogen and synthesize fatty acids, stimulates the uptake of amino acids, inhibits the breakdown of fat in adipose tissue, and stimulates the uptake of potassium into cells. People with T1DM require life-long insulin replacement therapy. Without insulin, diabetic ketoacidosis (DKA) develops and is life-threatening.[rx][rx]
Type 2 Diabetes Mellitus
- Type 2 diabetes mellitus (T2DM) accounts for around 90% of all cases of diabetes. In T2DM, the response to insulin is diminished, and this is defined as insulin resistance. During this state, insulin is ineffective and is initially countered by an increase in insulin production to maintain glucose homeostasis, but over time, insulin production decreases resulting in T2DM. T2DM is most commonly seen in persons older than 45 years, but it is increasingly seen in children, adolescents, and younger adults due to rising levels of obesity, physical inactivity, and energy-dense diets.
Gestational Diabetes Mellitus
- Hyperglycaemia which is first detected during pregnancy is classified as gestational diabetes mellitus (GDM), also known as hyperglycemia in pregnancy. Although it can occur anytime during pregnancy, GDM generally affects pregnant women during the second and third trimesters. According to American Diabetes Association (ADA), GDM complicates 7% of all pregnancies. Women with GDM and their offspring have an increased risk of developing type 2 diabetes mellitus in the future.
- GDM can be complicated by hypertension, preeclampsia, and hydramnios and may also lead to increased operative interventions. The fetus can have increased weight and size (macrosomia) or congenital anomalies. Even after birth, such infants may have respiratory distress syndrome, and subsequent childhood and adolescent obesity. Older age, obesity, excessive gestational weight gain, history of congenital anomalies in previous children, or stillbirth, or a family history of diabetes are risk factors for GDM.
Monogenic Diabetes
- A single genetic mutation in an autosomal dominant gene causes this type of diabetes. Examples of monogenic diabetes include conditions like neonatal diabetes mellitus and maturity-onset diabetes of the young (MODY). Around 1% to 5% of all diabetes cases are due to monogenic diabetes. MODY is a familial disorder and usually presents under age of 25 years.
Secondary Diabetes
- Secondary diabetes is caused due to the complication of other diseases affecting pancreas (for example, pancreatitis), hormone disturbances (for example, Cushing’s disease), or due to drugs (for example, corticosteroids).
Etiologic classification of diabetes mellitus
Type 1 diabetes (β-cell destruction, usually leading to absolute insulin deficiency)
-
Immune-mediated
-
Idiopathic
Other specific types
-
Chromosome 12, HNF-1α (MODY3)
-
Chromosome 7, glucokinase (MODY2)
-
Chromosome 20, HNF-4α (MODY1)
-
Chromosome 13, insulin promoter factor-1 (IPF-1; MODY4)
-
Chromosome 17, HNF-1β (MODY5)
-
Chromosome 2, NeuroD1 (MODY6)
-
Mitochondrial DNA
-
Others
-
Type A insulin resistance
-
Leprechaunism
-
Rabson-Mendenhall syndrome
-
Lipoatrophic diabetes
-
Others
-
Pancreatitis
-
Trauma/pancreatectomy
-
Neoplasia
-
Cystic fibrosis
-
Hemochromatosis
-
Fibrocalculous pancreatopathy
-
Others
-
Acromegaly
-
Cushing’s syndrome
-
Glucagonoma
-
Pheochromocytoma
-
Hyperthyroidism
-
Somatostatinoma
-
Aldosteronoma
-
Others
-
Vacor
-
Pentamidine
-
Nicotinic acid
-
Glucocorticoids
-
Thyroid hormone
-
Diazoxide
-
β-adrenergic agonists
-
Thiazides
-
Dilantin
-
γ-Interferon
-
Others
-
Congenital rubella
-
Cytomegalovirus
-
Others
-
“Stiff-man” syndrome
-
Anti-insulin receptor antibodies
-
Others
-
Down syndrome
-
Klinefelter syndrome
-
Turner syndrome
-
Wolfram syndrome
-
Friedreich ataxia
-
Huntington chorea
-
Laurence-Moon-Biedl syndrome
-
Myotonic dystrophy
-
Porphyria
-
Prader-Willi syndrome
-
Others
- Patients with any form of diabetes may require insulin treatment at some stage of their disease. Such use of insulin does not, of itself, classify the patient.
Other Types of Diabetes Mellitus
Monogenic Diabetes
- Characterization of the genetic etiology of diabetes enables more appropriate treatment, better prognosis, and counseling[rx]. Monogenic diabetes is due to a genetic defect in single genes in pancreatic β cells which results in disruption of β cell function or a reduction in the number of β cells. Conventionally, monogenic diabetes is classified according to the age of onset as neonatal diabetes before the age of six months or Maturity Onset Diabetes of the Young (MODY) before the age of 25 years. However, certain familial defects are manifested in neonatal diabetes, MODY or adult-onset diabetes[x,rx,rx].
- Others believe that the classification of diabetes as MODY and neonatal diabetes is obsolete and monogenic diabetes is currently used relating specific genetic etiologies with their specific treatment implications[rx]. Beta cell differentiation depends on the expression of the homeodomain transcription factor PDX1 where a mutation in the gene results in early-onset diabetes (MODY) and its expression decreases before the onset of diabetes[rx].
- The angiopoietin-like protein 8 (ANGPTL8) may represent a potential “betatrophin” that acts to promote the proliferation of beta cells, however, studies using mice lacking the ANGPTL8 active gene or overexpressed protein indicated that it did not seem to play a role in beta cells proliferation[rx].
- Mitochondrial diabetes is due to a point mutation in the mitochondrial DNA associated with deafness and maternal transmission of the mutant DNA can result in maternally-inherited diabetes[rx,rx].
Disease of the Exocrine Pancreas
- Damage of the β cells of the pancreas due to diffused injury of the pancreas can cause diabetes. This damage could be due to pancreatic carcinoma, pancreatitis, infection, pancreatectomy, and trauma[rx]. Atrophy of the exocrine pancreas leads to progressive loss of the β cells[rx].
- Accumulation of fat in the pancreas or pancreatic steatosis could lead to diabetes due to decreased insulin secretion but may require a long time before the damage to β cells occurs[rx]. In most cases, extensive damage of the pancreas is required before diabetes occurs and the exocrine function of the pancreas is decreased in these patients[rx]. Cirrhosis in cystic fibrosis may contribute to insulin resistance and diabetes[rx].
Hormones and Drugs
- Diabetes has been found in patients with endocrine diseases that secrete excess hormones like growth hormone, glucocorticoids, glucagon and epinephrine in certain endocrinopathies like acromegaly, Cushing’s syndrome, glucagonoma, and pheochromocytoma, respectively[rx]. Some of these hormones are used as drugs such as glucocorticoids to suppress the immune system and in chemotherapy and growth hormone to treat children with stunted growth.
Genetic Syndromes
- Diabetes has been detected in patients with various genetic syndromes such as Down syndrome, Klinefelter syndrome, Turner syndrome and Wolfram syndrome[rx].
Staging of Type 1 DM [4b]
[stextbox id=’grey’]
| Stage 1 | Stage 2 | Stage 3 | |
| Phenotypic characteristics | -Autoimmunity -Normoglycemia -Presymptomatic |
-Autoimmunity -Dysglycemia -Presymptomatic |
-New onset Hyperglycemia -Symptomatic |
| Diagnostic criteria | -2 or more islet autoantibodies -No impaired glucose tolerance or impaired fasting glucose |
-2 or more islet autoantibodies -Dysglycemia: impaired fasting glucose and/or impaired glucose tolerance: FPG 100-125mg/dl and/or 2-hour plasma glucose 140-199mg/dl A1C 5.7-6.4% or a ≥10% increase in A1C |
-Clinical symptoms -Diabetes by standard create |
“Type 3 diabetes” has been suggested as a term for Alzheimer’s disease as the underlying processes may involve insulin resistance by the brain.[rx]
[/stextbox]
Causes of Diabetes Mellitus
- The family history of diabetes
- African-American, Hispanic, Native American, or Asian-American race, Pacific Islander or ethnic background
- Being overweight
- Physical stress (such as surgery or illness)
- Use of certain medications, including steroids
- Injury to the pancreas (such as infection, tumor, surgery or accident)
- Autoimmune disease
- High blood pressure
- Abnormal blood cholesterol or triglyceride levels
- Age (risk increases with age)
- Smoking
- History of gestational diabetes
- Acromegaly
- In acromegaly
- Aging process
- In human aging: Endocrine system
- Congenital disorders
- In congenital disorder: Growth defects
- Diet
- In nutritional disease: Diabetes mellitus and metabolic disorders
- Elevated blood sugar level
- In blood: Laboratory examination of blood
- Hyperglycemia
- In hyperglycemia
- Insulin deficiency
- In insulin
- In islets of Langerhans
- Metabolic disorders
- In hormone: Growth hormone (somatotropin)
- In disease: Metabolic defects
- In metabolic disease: Metabolic pathways
- Pancreatitis
- In pancreatitis
It is important to note that sugar itself does not cause diabetes. Eating a lot of sugar can lead to tooth decay, but it does not cause diabetes.
The following is a comprehensive list of other causes of diabetes:[rx]
[dropshadowbox align=”none” effect=”lifted-both” width=”auto” height=”” background_color=”#ffffff” border_width=”1″ border_color=”#dddddd” ]
Genetic defects of β-cell function
Genetic defects in insulin processing or insulin action
Exocrine pancreatic defects
|
Endocrinopathies
Infections
Drugs
|
[/dropshadowbox]
A 2018 study suggested that three types should be abandoned as too simplistic.[rx] It classified diabetes into five subgroups, with what is typically described as type 1 and autoimmune late-onset diabetes categorized as one group, whereas type 2 encompasses four categories. This is hoped to improve diabetes treatment by tailoring it more specifically to the subgroups.[ rx]
Symptoms of Diabetes Mellitus
If type 2 diabetes goes untreated, blood sugar levels stay high all the time. This isn’t always noticeable at first. Type 2 diabetes can develop gradually over several years without any noticeable symptoms. Blood sugar levels that are always too high may cause the following symptoms, though
- In Type 1 diabetes, the classic symptoms are excessive secretion of urine (polyuria), thirst (polydipsia), weight loss and tiredness.
- These symptoms may be less marked in Type 2 diabetes. In this form, it can also happen that no early symptoms appear and the disease is only diagnosed several years after its onset, when complications are already present.
- Increased thirst
- Increased hunger (especially after eating)
- Dry mouth
- Frequent urination
- Unexplained weight loss (even though you are eating and feel hungry)
- Weak, tired feeling
- Blurred vision
- Numbness or tingling in the hands or feet
- Slow-healing sores or cuts
- Dry and itchy skin
- Frequent yeast infections or urinary tract infections
- Presence of ketones in the urine (ketones are a byproduct of the breakdown of muscle and fat that happens when there’s not enough available insulin)
- Fatigue
- Irritability
- Slow-healing sores
- Frequent infections, such as gums or skin infections and vaginal infections
- Extreme thirst
- Tiredness and listlessness
- Nausea
- Dizziness
If someone has extremely high blood sugar levels, they may feel confused and drowsy or even lose consciousness (diabetic coma).
Diagnosis of Diabetes Mellitus
Regular appointments with the primary care physician and a certified diabetes educator are some of the best things a patient can do in the early weeks after a diagnosis of diabetes. Upon the diagnosis of diabetes, the primary care physician, specialist, or endocrinologist will conduct a full physical and medical examination. A thorough assessment covers topics such as:
Medical History
- The family history of diabetes, cardiovascular disease, and stroke
- Eating and exercise habits; growth and development of children and adolescents
- Diabetes education history
- Review of previous treatment regimen and response to therapy (HbA1c records)
- A list of current medications, including:
- Prescription medications
- Over-the-counter medications
- Vitamin, mineral or herbal supplements
- Smoking history, including encouragement of smoking cessation (if applicable)
- Current treatment plan, including medications, medication compliance and barriers, meal plan, physical activity patterns, readiness for behavior change
- Results of glucose monitoring and patient’s use of data
- Diabetic ketoacidosis frequency, severity, and cause
- Hypoglycemic episodes and awareness
- History of diabetes-related complications
- Microvascular: retinopathy, nephropathy, neuropathy
- Macrovascular: coronary artery disease, cerebrovascular disease, peripheral artery disease
- Urination abnormalities, which can indicate kidney disease
- Signs of complications with pregnancy or trying to get pregnant for women patients
Physical examination
- Height, weight, body mass index
- Blood pressure measurements
- Funduscopy
- Thyroid palpation
- Skin examination at insulin injection sites
- The comprehensive examination of hands, fingers, feet, and toes for circulatory abnormalities
Additional laboratory evaluation
- If results not available within the past 3 months
- HbA1c
If results not available within the past year
- Fasting lipid profile: including total, LDL, HDL cholesterol and triglycerides
- Liver function test
- Test for urine albumin excretion with spot urine albumin/creatinine ratio
- The thyroid-stimulating hormone in type 1 diabetes, dyslipidemia, or women over 50 years old
Referrals
- Eye care profession for annual dilated fundus examination
- Family planning for women of reproductive age
- Registered dietitian for medical nutrition therapy
- Diabetes self-management education (DSME)
- Dentist for the comprehensive periodontal exam
- Mental health professional if needed
[stextbox id=’info’]
| “One- Step” Diagnosis- 75-gram glucose tolerance test (IADPSG Consensus) | |||
|---|---|---|---|
|
PLASMA GLUCOSE* | ||
|
≥92 mg/dl (5.1 mmol/L) | ||
|
≥180 mg/dl (10.0mmol/L) | ||
|
≥153 mg/dl (8.5 mmol/L) | ||
| “Two-Step” Diagnosis- (NIH Consensus) | |||
| Step 1: Perform a 50-gram glucose load test (nonfasting) | |||
|
PLASMA GLUCOSE | ||
|
≥140 mg/dl (7.8 mmol/L) | ||
| IF POSITIVE, STEP 2: 100-gram glucose tolerance test | |||
| Carpenter/Coustan | NDDG | ||
|
PLASMA GLUCOSE+ | TIME | PLASMA GLUCOSE+ |
|
≥95 mg/dl (5.3 mmol/L) | Fasting | ≥105 mg/dl (5.8 mmol/L) |
|
≥180 mg/dl (10.0 mmol/L) | 1-hour | ≥190 mg/dl (10.6 mmol/L) |
|
≥155 mg/dl (8.6 mmol/L) | 2-hour | ≥165 mg/dl (9.2 mmol/L) |
|
≥140 mg/dl (7.8 mmol/L) | 3-hour | ≥145 mg/dl (8.0 mmol/L) |
| *One abnormal value is sufficient to make the diagnosis of GDM. The test should be done in the morning after at least 8 hour fast. +Two abnormal values establish the diagnosis of GDM. NDDG=National Diabetes Data Group. | |||
Diabetes can be diagnosed either by A1C criteria or plasma glucose concentration (fasting or 2-hour plasma glucose).
[/stextbox]
Fasting Plasma Glucose (FPG)
- A blood sample is taken after an 8 hour overnight fast. As per ADA, FPG level of more than 126 mg/dL (7.0 mm/L) is consistent with the diagnosis.
Two-Hour Oral Glucose Tolerance Test (GTT)
- In this test, the plasma glucose level is measured before and 2 hours after ingestion of 75 gm of glucose. DM is diagnosed if plasma glucose (PG) level in the 2-hour sample is more than 200 mg/dL (11.1 mmol/L). It is also a standard test but is inconvenient and more costly than FPG and has major variability issues. Patients need to consume a diet with at least 150 g per day of carbohydrate for 3 to 5 days and not take any medications that can impact glucose tolerance such as steroids and thiazide diuretics.
Glycated Hemoglobin (A1C)
- This test gives an average of blood glucose over the last 2 to 3 months. Patients with A1C greater than 6.5% (48 mmol/mol) are diagnosed as having DM. A1C is a convenient, rapid, standardized test and shows less variation due to pre-analytical variables. It is not much affected by acute illness or stress.
- A1C is costly and has many issues as discussed below including lower sensitivity. A1C should be measured using the National Glycohemoglobin Standardization Program (NGSP) certified method standardized to Diabetes Control and Complications Trial (DCCT) assay. It is affected by numerous conditions such as sickle cell disease, pregnancy, hemodialysis, blood loss or transfusion, or erythropoietin therapy. It has not been well validated in non-Caucasian populations.
- Anemia due to deficiency of iron or vitamin B12 leads to spurious elevation of A1C, limiting its use in countries with high prevalence of anemia. Also, in children and elderly, the relation between A1C and FPG is suboptimal.
- For all of the above tests, if the person is asymptomatic, testing should be repeated later to make a diagnosis of diabetes. FPG, 2-hour PG during 75-g GTT, and A1C are equally appropriate for diagnosis of DM. There is no concordance between the results of these tests.
Diagnosis of Gestational Diabetes Mellitus
- Pregnant women not previously known to have diabetes should be tested for GDM at 24 to 28 weeks of gestation. ADA and ACOG recommend using either a 1-step or 2-step approach for diagnosing GDM.
One-Step Strategy
- 75 gm OGTT is performed after an overnight fast. Blood samples are collected at fasting for 1 hour, and 2 hours. GDM is diagnosed if fasting glucose meet or exceed 92 mg/dl (5.1 mmol/l), 1-hour serum glucose of 180 mg/dl (10.0 mmol/l) or 2-hour serum glucose of 153 mg/dl (8.5 mmol/l).
Two-Step Strategy
-
Step one: Perform 50-gram glucose challenge test irrespective of last meal. If PG at 1-hour after the load is ≥ 140mg/dl (7.8 mmol/l), proceed to step 2.
-
Step 2: 100 g glucose OGTT is performed after overnight fasting. Cut off values are fasting PG 95 or 105 mg/dl (5.5/5.8 mmol/l), 1-hour PG of 180 or 190 mg/dl (10.0/10.6 mmol/l), 2-hour PG of 155 or 165 mg/dl (8.6/9.2 mmol/l) or 3-hour PG of 140 or 145 mg/dl (7.8/8.0 mmol/l). GDM is diagnosed if 2 or more PG levels equal or exceed these cutoffs.
Treatment of Diabetes Mellitus
[stextbox id=’info’]
Classification of Antidiabetic Drugs
|
Oral anti-diabetic drugs, insulins and insulin analogs, and other drugs used in diabetes (A10)
|
|||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Insulin |
|
||||||||||||||||||||||||
| Other |
|
||||||||||||||||||||||||
|
|||||||||||||||||||||||||
[/stextbox]
Pharmacological Agents
Biguanides
- Biguanides, of which metformin is the most commonly used in overweight and obese patients, suppresses hepatic glucose production, increases insulin sensitivity, enhances glucose uptake by phosphorylating GLUT-enhancer factor, increases fatty acid oxidation, and decreases the absorption of glucose from the gastrointestinal tract.[rx]
- Research published in 2008 shows the further mechanism of action of metformin as activation of AMP-activated protein kinase, an enzyme that plays a role in the expression of hepatic gluconeogenic genes.[rx] Due to the concern of development of lactic acidosis, metformin should be used with caution in elderly diabetic individuals with renal impairment. It has a low incidence of hypoglycemia compared to sulfonylureas.[rx]
Sulfonylureas
- These generally well tolerated but because they stimulate endogenous insulin secretion, they carry a risk of hypoglycemia.[rx] Elderly patients, with DM who are treated with sulfonylureas, have a 36% increased risk of hypoglycemia compared to younger patients.[rx] Glyburide is associated with higher rates of hypoglycemia compared to glipizide.[rx]
- Some of the risk factors for hypoglycemia are age-related impaired renal function, simultaneous use of insulin or insulin sensitizers, age greater than 60 years, recent hospital discharge, alcohol abuse, caloric restriction, multiple medications or medications that potentiate sulfonylurea actions.[rx] Use of long-acting sulfonylurea such as glyburide should be avoided in elderly patients with DM and use of short-acting glipizide should be preferred.[rx]
Meglitinides
- Repaglinide and nateglinide are non-sulfonylurea secretagogues which act on the ATP-dependent K-channel in the pancreatic beta cells thereby stimulating the release of insulin from the beta cells, similar to sulfonylurea, though the binding site is different.[rx]
- Meglitinides have a rapid onset and a short duration of action (4-6 hrs) and thus lower risk of hypoglycemia. Meglitinides are given before meals for postprandial blood glucose control. Pre-prandial administration allows flexibility in case a meal is missed without increased risk of hypoglycemia.[rx]
- Repaglinide is mainly metabolized in the liver with very minimal amounts excreted via the kidneys and thus dose adjustment is not necessary for patients with renal insufficiency except those with end-stage renal disease.[rx]
Thiazolidinediones
- Thiazolidinedione is an insulin sensitizer, selective ligands transcription factor peroxisomes proliferator-activated gamma. They are the first drugs to address the basic problem of insulin resistance in type 2 DM patients,[rx] whose class now includes mainly pioglitazone after the restricted use of rosiglitazone recommended by Food and Drug Administration (FDA) recently due to increased cardiovascular events reported with rosiglitazone.[rx]
- Pioglitazone use is not associated with hypoglycemia and can be used in cases of renal impairment and thus well tolerated in older adults. On the other hand, due to concerns regarding peripheral edema, fluid retention and fracture risk in women, its use can be limited in older adults with DM. Pioglitazone should be avoided in elderly patients with congestive heart failure and is contraindicated in patients with class III-IV heart failure.[rx]
Alpha-Glucosidase Inhibitors
- Acarbose, Voglibose, and Miglitol have not widely been used to treat type 2 DM individuals but are likely to be safe and effective. These agents are most effective for postprandial hyperglycemia and should be avoided in patients with significant renal impairment. Their use is usually limited due to high rates of side-effects such as diarrhea and flatulence.[rx]
- Voglibose, which is the newest of the drugs, has been shown in a study to significantly improve glucose tolerance, in terms of delayed disease progression and in the number of patients who achieved normoglycemia.[rx]
Incretin-Based Therapies
- Glucagon-like peptide 1 (GLP-1) analogs are the foundation of incretin-based therapies which are to target this previously unrecognized feature of DM pathophysiology resulting in sustained improvements in glycemic control and improved body weight control.[rx]
- They are available for use as monotherapy, as an adjunct to diet and exercise or in combination with oral hypoglycemic agents in adults with type 2 DM. Examples are Exenatide, an incretin mimetic, and Liraglutide.[rx]
- There is no risk of hypoglycemia with the use of GLP-1 therapies (unless combined with insulin secretagogues). In addition, emerging evidence suggests incretin-based therapies may have a positive impact on inflammation, cardiovascular and hepatic health, sleep, and the central nervous system.[rx]
Dipeptidyl-Peptidase IV Inhibitors
- Dipeptidyl-peptidase (DPP) IV inhibitors inhibit dipeptidyl peptidase-4 (DPP-4), a ubiquitous enzyme that rapidly inactivates both GLP-1 and GIP, increase activity levels of these hormones and, in doing so, improves islet function and glycemic control in type 2 DM.[rx]
- DPP-4 inhibitors are a new class of anti-diabetogenic drugs that provide comparable efficacy to current treatments. They are effective as monotherapy in patients inadequately controlled with diet and exercise and as add-on therapy in combination with metformin, thiazolidinediones, and insulin.
- The DPP-4 inhibitors are well tolerated, carry a low risk of producing hypoglycemia and are weight neutral. However, they are relatively expensive.[rx] The long-term durability of effect on glycemic control and beta-cell morphology and function remain to be established.[rx],[rx]
Insulin
- Insulin is used alone or in combination with oral hypoglycemic agents. Augmentation therapy with basal insulin is useful if some beta cell function remains. Replacement of basal-bolus insulin is necessary if beta cell exhaustion occurs. Rescue therapy using replacement is necessary in cases of glucose toxicity which should mimic the normal release of insulin by the beta cells of the pancreas.[rx]
- Insulin comes in injectable forms – rapid acting, short acting, intermediate acting, and long-acting. The long acting forms are less likely to cause hypoglycemia compared to the short acting forms.
Insulin Analogs
- Insulin therapy was limited in its ability to mimic normal physiologic insulin secretion. Traditional intermediate- and long-acting insulins (NPH insulin, Lente insulin, and ultralente insulin) are limited by inconsistent absorption and peaks of action that may result in hypoglycemia.[rx],[rx]
- The pharmacokinetic profiles of the new insulin analogs are distinct from those of the regular insulins, and their onset and duration of action range from rapid to prolonged. Currently, two rapid-acting insulin analogs, insulin lispro, and insulin aspart, and one long-acting insulin analog, insulin glargine, are available.[rx],[rx]
Dipeptidyl peptidase-4 inhibitors
- The incretin agents (GLP1 and GIP), secreted by intestine L cells, increase insulin secretion and inhibit glucagon in response to nutrient inputs. The glucoregulatory effects of incretins are the basis for treatment with inhibitors of DPP4 in patients with T2DM. Agents that inhibit DPP4, an enzyme that rapidly inactivates incretins, increase activity levels of these hormones and, in doing so, improve islet function and glycaemic control in T2DM.
Sitagliptin
- Sitagliptin, which is approved for the treatment of T2DM in many countries, can be employed alone or dual therapy with a sulfonylurea, metformin or TZD or third therapy. The normal dose of sitagliptin is 100 mg once daily; the half dose is utilized in patients with an eGFR 30-50 mL/min, and quarter dose in those with an eGFR < 30 mL/min[rx]. Monotherapy with this drug there is multiple studies, with a significant reduction in HbA1c. The results of a study with sitagliptin monotherapy for 18 wk were: HbA1c significantly decreased with sitagliptin 100 and 200 mg compared to placebo (low HbA1c vs placebo: -0.48% and -0.60% respectively). Sitagliptin also significantly reduced fasting blood glucose vs placebo [rx].
Vildagliptin
- This is an iDPP4 which FDA was not approved so that is not being used in the United States. The usual dose is 50 mg twice daily when utilized as monotherapy, with metformin, or with a TZD, and 50 mg once daily (in the morning) when utilized with a sulfonylurea. No dose adjustment is necessary in patients with mild renal impairment (creatinine clearance ≥ 50 mL/min). In patients with moderate or severe renal impairment, the dose is 50 mg once daily[rx].
Saxagliptin
- Saxagliptin is approved as a drug for home treatment of T2DM or dual therapy for patients not controlled with a sulfonylurea, metformin or TZD. The dose is 2.5 or 5 mg of saxagliptin once daily. The dose of 2.5 mg is recommended for patients with an eGFR ≤ 50 mL/min and patients taking drugs inhibitors of cytochrome P450 3A4/5 (e.g., ketoconazole), Saxagliptin monotherapy is effective, achieving reductions in HbA1c of 0.5 in naive patients vs placebo[rx,rx].
- There are studies with saxagliptin (2.5, 5 and 10 mg) in dual therapy with metformin showed a statistically significant adjusted mean HbA1c decrease from baseline to week 24 compared to placebo (-0.59%, -0.69%, and -0.58% vs +0.13%; all P < 0.0001)[rx]. There are also studies showing the efficacy of sitagliptin in combination with sulfonylureas and TZD.
Linagliptin
- The dose of linagliptin is 5 mg once daily. It is eliminated mainly through the enterohepatic system so it is not necessary to adjust the dose in patients with renal or hepatic impairment. Inducers of CYP3A4 or P-glycoprotein (e.g., rifampicin) may reduce the effectiveness of this agent. In patients receiving these drugs should avoid the use of linagliptin.
- In a monotherapy study vs placebo, linagliptin achieved a reduction in HbA1c of 0.44% against rising 0.25% with placebo in 6 mo[rx]. In a 24 wk study in triple therapy in patients treated with metformin and sulfonylureas that was added linagliptin or placebo, appeared a reduction in HbA1c of 0.72% in the group with linagliptin vs 0.1% in the group with placebo[rx].
Alogliptin
- The usual dose of alogliptin is 25 mg once daily, with dose reductions to 12.5 mg once daily in patients with creatinine clearance between 30 and 60 mL/min and to 6.25 mg daily in patients with creatinine clearance < 30 mL/min or undergoing dialysis[rx].
- In a study to twelve weeks in patients treated with metformin with poor control of their diabetes, alogliptin group achieved a reduction in HbA1c of 0.64% compared to an increase of 0.22% in the placebo group[rx]. In another 26 wk studies, with alogliptin (12.5 or 25 mg once a day) vs placebo in patients with poorly controlled T2DM on a stable dose of glyburide (n = 500) or insulin (alone or in combination with metformin, n = 390) there were greater reductions in HbA1c in the alogliptin groups (mean change in HbA1c from baseline -0.39, -0.53 and +0.01 percentage points for the 12.5, 25 mg, and placebo groups, respectively, in the glyburide trial, and -0.63, -0.71 and -0.13 percentage points, respectively, in the insulin trial)[rx,rx].
Sodium-Glucose cotransporter-2 Inhibitor
- iSGLT2 inhibit renal reabsorption of glucose, increase its excretion and reduce hyperglycemia in patients with T2DM. Therefore, reducing the reabsorption of glucose by the inhibition of SGLT2 is a new way to treat T2DM. The increase in glucosuria and diuresis produced results in a reduction in weight and blood pressure[rx].
- Kidneys from healthy people filter approximately 180 g of glucose each day through renal glomerulus and reabsorbed in the then proximal convoluted tubule. This is possible by passive and active co-carriers which are known as glucose transporter (GLUT) and SGLT[rx] conveyors.
- There are two types of SGLT; SGLT1 located mainly in the small intestine and the kidney proximal convoluted tubule, and SGLT2 located only in the proximal tubule (segment 1 and 2), that are responsible for about 90% of glucose reabsorption[rx]. The other 10% of the glucose is reabsorbed by SGLT1 in segment 3. SGLT2 inhibitors block the SGLT2 transporter in the proximal tubule, to lower glucose reabsorption and increase its excretion in the urine. Glucose is excreted in the urine and plasma levels are reduced by improving glycemia figures plasma[rx–rx].
- It is an independent mechanism of insulin, there is low risk for hypoglycemia, and no risk of fatigue or overstimulation of the beta cells[rx]. Due to its mode of action is based on normal glomerular-tubular function; the iSGLT2 efficiency is lower in patients with renal failure[rx]. The three most representative drugs family iSGLT2 are Dapagliflozin, canagliflozin, and empagliflozin.
Dapagliflozin
- Dapagliflozin was the first iSGLT2 employee and has many published data from clinical trials. In phase 3 trials comparing placebo for 24 wk and dapagliflozin (2.5, 5 and 10 mg once daily) used alone or added to metformin[rx], pioglitazone[rx], glimepiride[rx] or insulin[rx] was observed that HbA1c and fasting plasma glucose in patients with T2DM was reduced. In tests longer-term (102 wk) added to metformin, dapagliflozin resulted in a sustained decrease in HbA1c, glucose fasting blood glucose and weight without increasing the risk of hypoglycemia in patients with T2DM not controlled on metformin alone[rx].
- The initial decrease in HbA1c observed at 24 wk with both doses of dapagliflozin (5 or 10 mg) added to metformin was maintained at 102 wk, and was superior to placebo (-0.58%, -0.78% and 0.02% against). Also, the low fasting plasma glucose with both doses of dapagliflozin remained and was higher than placebo (-1.47 mmol/L and -1.36 mmol/L vs -0.58 mmol/L). This drug has studies which compared with patients whose hyperglycemia glipizide was poorly controlled by metformin[rx].
- After 52 wk, a drop in HbA1c starting from the baseline of -0.52% is a target with dapagliflozin (≤ 10 mg/d) and glipizide (≤ 20 mg/d). Weight reduction was greater with dapagliflozin (-3.2 kg) vs glipizide (+1.4 kg). Dapagliflozin (≤ 10 mg/d) in T2DM patients was non-inferior to glipizide (≤ 20 mg/d) in reduction of HbA1c at 52 wk (both -0.52%). At 4 years the HbA1c reduction is attenuated in both groups, but more in the glipizide vs dapagliflozin (+0.2% vs -0.1%). There were differences in weight change, with weight loss in the dapagliflozin group vs weight gain in the glipizide group (-3.95 kg vs +1.12 kg). In the dapagliflozin group decreases the mean average of systolic blood pressure, but did no change in the glipizide group (difference: -3.7 mmHg)[rx].
Canagliflozin
- Canagliflozin was the first of this family of drugs approved by the FDA and began its commercialization in March 2013 for use in T2DM. It is an effective drug in monotherapy and after 26 wk of treatment with canagliflozin 100 mg and 300 mg once daily significantly reduced HbA1c (-0.77% and -1.03% respectively) in patients with T2DM not controlled with diet and exercise compared to placebo (0.14%, P < 0.001)[rx].
Empagliflozin
- Empagliflozin is a drug that has eight multinational clinical trials, including a very important safety trial of cardiovascular risk. Data empagliflozin 12 wk at doses 5-25 mg/d are increased excretion of glucose and a decrease of fasting blood glucose (-31.1 mg/dL. at 25 mg vs an increase +0.8 mg/dL. placebo), HbA1c (-0.63% vs 25 mg vs an increase of +0.09%) and body weight (-2.0 kg to 25 mg vs -0.8 kg) in T2DM[rx].
- Both doses of empagliflozin (10 mg or 25 mg daily) added to metformin received greater reductions in HbA1c vs sitagliptin (-0.34% to -0.63% vs -0.40%) and these were maintained for 90 wk. The fasting glucose reduction was also higher after 90 wk of treatment with two doses of empagliflozin against sitagliptin (-21 mg/dL and -32 mg/dL vs -16 mg/dL), and these effects were maintained over the treatment period[rx].
- The weight was reduced from the baseline of -2.2 to -4.0 kg with empagliflozin, -1.3 kg with metformin, and sitagliptin -0.4 kg after 90 wk[rx]. In a randomized, double-blind empagliflozin (10, 25 mg) or placebo add-on to basal insulin for 78 wk; compared with placebo, 10 and 25 mg/d of empagliflozin significantly lower body weight (-2.2 kg, -2.0 kg, and +0.7 kg respectively), and decreased HbA1c (-0.48%, -0.64%, and -0.02%, respectively), and systolic blood pressure (-4.1 mmHg, -2.4 mmHg, and +0.1 mmHg, respectively)[rx]. Therefore, a long-term empagliflozin is an effective treatment for patients with T2DM.
Future in Drug Therapy Inhaled Insulin
- The inhaled form of rapidly acting insulin which became available in 2006,[rx] after it was approved by both the European Medicines Evaluation Agency and FDA for treatment of type 1 and type 2 DM in adults.[rx]–[rx] It is a rapid-acting form of insulin that was indicated for use in adults with type 1 and type 2 DM and has the advantage of delivery directly into the lungs. Studies have however shown that inhaled insulin is as effective as, but not better than short acting insulin.[rx] It was withdrawn from the market by the manufacturer in October 2007 due to poor sales.
Bromocriptine
- Quick-release bromocriptine has recently been developed for the treatment of type 2 DM. However, the mechanism of action is not clear. Studies have shown that they reduce the mean HbA1c levels by 0.0% to 0.2% after 24 weeks of therapy.[rx]
Insulin secretagogues: Sulfonylureas and meglitinides
- Due to their efficacy, long experience use, and low cost, sulfonylureas are widely used in the general population. They are usually well-tolerated drugs even in the elderly. However, hypoglycemia is the most common and the most dangerous side effect.
- Hypoglycemia is more common with long-acting sulfonylurea drugs such as chlorpropamide, glyburide, and glimepiride. Those medications should be avoided in elderly especially if they have diarrhea, they are addicted to alcohol and have memory troubles; situations that increase the risk for hypoglycemia and weight gain.
- Short action-acting sulfonylureas such as meglitinides are preferable in elderly because of their low rate of hypoglycemia, but they have the same risk for weight gain.
Thiazolidinediones
- The thiazolidinediones such as rosiglitazone and especially pioglitazone improve insulin resistance and may improve insulin secretion in response to glucose in people with reduced glucose tolerance.
- Actually, pioglitazone is now the only marketed product that can be used as a good alternative for older people due to its low-risk for hypoglycemia. It can be used alone or in association with metformin. Its main side effect is fluid retention. Therefore, it is not suitable for patients with congestive heart failure.
- Glitazones require 2–4 weeks to exert their full anti-hyperglycemic effect. Therefore, they can be used in a patient with lower initial HbA1c and those who are allergic to sulfonylureas, or those not willing to use insulin.
- Although they are well-tolerated in old people and can be given in renal insufficiency, their high cost and problems regarding fluid retention increased the incidence of fractures (because of bone loss), and bladder cancer limits their usefulness.
Alpha-Glucosidase Inhibitors
- Alpha-glucosidase inhibitors (AGI) (acarbose and miglitol) are products that inhibit the gastrointestinal alpha-glucosidases which are enzymes converting carbohydrates into monosaccharides. Consequently, they reduce the rise in postprandial blood glucose after meals.
- AGI can be used alone or in combination with metformin, sulfonylurea or insulin. However, they are not widely tested in older diabetic patients, although they are likely to be safe and efficient. The main side effects are gastrointestinal troubles such as flatulence and diarrhea, which are a limitation of their use.
Incretin-Based Therapies
- Dipeptidylpeptidases-4 (DPP-4) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists seem to be very interesting drugs for elderly as they are associated to low hypoglycemic risk when used alone or as add-on therapy to metformin.[rx]
- DPP-4 inhibitors are deemed to be relatively weak agents lowering blood glucose through several mechanisms when used alone or at add-on therapy with metformin, sulfonylurea, and thiazolidinediones. They have no risk of hypoglycemia and are weight-neutral. Therefore, they may be attractive agents to use in older adults, but long-term safety is not proved yet, and their price is relatively high.
- Furthermore, their dose should be adjusted in kidney insufficiency, although, Halimi et al.’s study showed the efficacy and safety of DPP-4 inhibitors in the elderly even in the presence of renal impairment.[rx] On another hand Shankar et al. have recently demonstrated that in elderly and compared to sulfonylureas Sitagliptin has the same efficacy, but a lower risk for hypoglycemia and was accompanied with weight loss.[rx]
- GLP-1 agonists that include exenatide, liraglutide and recently lixisenatide may also be advantageous, as they do not increase hypoglycemic risk unless they are associated with sulfonylureas. They also cause weight loss and are interesting in over-weight or obese old patients.
- A pooled analysis of 06 randomized trials showed that liraglutide is effective and well-tolerated in old persons. However, liraglutide dosage needs to be adjusted according to kidney function.[rx] These agents require a period of 2–4 weeks for dose titration to reach their maximal effect. GLP-1 agonists may also have neuro-protective properties and may be useful in old patients with neurodegenerative diseases.[rx]
Sodium-glucose co-transporter type 2 inhibitors
- The Inhibitors of sodium-glucose co-transporter type 2 (SGLT2) such as canagliflozin and dapagliflozin represent a novel class of glucose-lowering agents that lower plasma glucose levels through pharmacological inhibition of glucose reuptake from the kidney.[rx] Compared to placebo, SGLT2 lower HbA1c by 0.5–0.8% when used as monotherapy or add-on therapy.[rx]
- SGLT2 inhibitors prescription is limited due to the high frequency of urinary and genital mycotic infections and because of other adverse effects including hypotension, dizziness, and renal function worsening. Serious adverse effects including severe hypoglycemia due to depletion of hepatic glycogen storage, acceleration of diabetes-associated sarcopenia, and ketoacidosis have been reported in some rare cases.[rx] Therefore, SGLT2 inhibitors should be used with caution in old people in the first category. However, they should be totally avoided in other categories, especially in people with chronic kidney diseases, sarcopenia, and risk of dehydration.[rx]
INJECTABLE AGENTS
RA-GLP1
- Human GLP1 is secreted in response to food intake and stimulates insulin release[rx]. Two incretins have been identified: GLP1, which is produced and released mainly by L-cells located in the distal ileum and GIP, which is secreted by enteroendocrine K-cells in the proximal gut.
- GLP1 treatment in T2DM patients increased insulin secretion glucose dependent and decrease secretion of glucagon, slowed gastric emptying, raised satiety, and reduce food intake[rx]. GLP1 also protect against myocardial ischemia[rx,rx]. In blood vessels promotes endothelium-independent artery relaxation protecting against endothelial dysfunction. Also have effect in protecting renal function by increasing diuresis and natriuresis[rx,rx]. All of these actions allow lower blood pressure and have positive effects on cardiovascular risk markers such as plasminogen activator inhibitor and brain natriuretic peptide.
Exenatide
- Exenatide was the first RA-GLP1 to be approved for glycaemic control. Is a synthetic 39-amino acid peptide identical to the exendine-4 molecule isolated from salivary glands of the Gila monster; shares approximately 53% homology with native GLP1. The usual dose is 5-10 μg twice-daily subcutaneous injection.
- Exenatide in monotherapy lowered HbA1c by 0.7%-0.9% and fasting plasma glucose by 17.5-18.7 mg/dL. The efficacy and safety of exenatide has been proved in several clinical studies[rx–rx].
Lixisenatide
- Lixisenatide is an RA-GLP1 that shares some structural elements with exendin-4. Compared with native GLP1, it has a prolonged half-life (2.7 to 4.3 h). Is available in Europe, not in the United States, for use in combination with oral agents or insulin; is not considered first-line therapy. Is available in a prefilled pen containing 14 doses of 10 or 20 mcg of lixisenatide. The initial dose is 10 mcg subcutaneously once daily within one hour prior to any meal of the day; after 2 wk the dose can be increased to 20 mcg.
- Lixisenatide has been studied as monotherapy and in combination with one or two oral agents (metformin, pioglitazone, sulfonylureas). In a 24-wk double-blind trial of lixisenatide 20 mcg once daily vs placebo in 680 T2DM patients inadequately controlled with metformin (mean HbA1c 8.1%), the mean reduction in HbA1c was significantly greater with lixisenatide (-0.9% vs -0.4%)[rx], and in another 24-wk no inferiority trial of once-daily subcutaneous lixisenatide 20 mcg once daily vs exenatide 10 mcg twice daily in 634 T2DM patients inadequately controlled with metformin alone (mean baseline HbA1c 8%), lixisenatide was no inferior to exenatide (mean change HbA1c -0.79% vs -0.96% with exenatide)[rx].
Liraglutide
- Liraglutide is a human RA-GLP1, obtained through modifications of the human GLP1, with a large half-life, which is administered once a day. Is available for use as monotherapy (adjunct to life style changes) or in combination with oral agents and basal insulin in adults with T2DM. The initial dose is 0.6 mg once daily subcutaneously the first week, and after the dose should be increased to 1.2 mg; and if HbA1c remain above the goal range the dose can be increased to 1.8 mg. It can be administered at any time of the day, with or without meals.
Exenatide LAR
- Administration of exenatide LAR was proved more effective than the highest dose of exenatide twice-daily[rx,rx], sitagliptin and pioglitazone[rx], and insulin glargine[rx] in T2DM patients treated with oral hypoglycaemic agents. Is available for use as an adjunct to lifestyle changes to improve glycaemic control in T2DM. The usual dose is 2 mg subcutaneously once weekly at any time of the day with or without meals.
Albiglutide
- It is an RA-GLP1 with a half-life of five to seven days, which allows once-weekly administration. It is available for use as monotherapy or in combination with oral agents or basal insulin. Is available in a prefilled pen that contains a powder (30 or 50 mg), and a diluent to make a solution that is injected subcutaneously once weekly. The initial dose is 30 mg, and if after 6-8 wk blood glucose remain above the goal, the dose can be increased to 50 mg.
- Albiglutide has been studied as monotherapy and in combination with one or two oral agents (metformin, pioglitazone, sulfonylureas, and insulin). As examples: In a one-year trial of albiglutide vs insulin glargine in 779 T2DM patients inadequately controlled with metformin (with or without a sulfonylurea), the mean HbA1c reduced from 8.28% to 7.62% in the albiglutide group and from 8.36% to 7.55% in the glargine group[rx].
Dulaglutide
- It is the last RA-GLP1 in appear. It has a structure that gives it the properties of slow absorption and reduced renal clearance rate. It is available for use as monotherapy or in combination with oral agents or insulin, in a ready-mixed pen at a dose of 0.75 mg in monotherapy once weekly or 1.5 mg in combination, once weekly.
OTHER TREATMENTS
Colesevelam
- Colesevelam is a bile acid sequestrant that reduces LDL cholesterol in patients with hypercholesterolemia. Possibly colesevelam interferes glucose absorption at gastrointestinal level. In T2DM patients not controlled, colesevelam added to the treatment of oral hypoglycaemic agents or insulin resulted in a reduction of HbA1c levels of 0.5%[rx–rx].
Bromocriptine
- Bromocriptine is a dopamine agonist that has been used for the treatment of hyperprolactinemia and Parkinson disease. The mechanism of action in reducing blood glucose is unknown. A quick release formulation of bromocriptine (Cycloset) was approved by the FDA for the treatment of T2DM[rx]. In short-term clinical trials in T2DM patients, bromocriptine (up to 4.8 mg daily) as monotherapy or added to sulfonylureas reduce HbA1c compared with placebo in 0.4%-0.5%[rx,rx].
Pramlintide
- Pramlintide is an amylin analog that is administered by mealtime subcutaneous injection. It is available for use for both T1 and insulin-treated T2DM; is only be used in patients also taking prandial insulin. Pramlintide replicates amylin actions and controls glucose without causing weight gain.
The Future Treatment of Diabetes
- Unfortunately, all anti-diabetic agents have adverse effects and are expensive. Therefore, the investigation of novel antidiabetic regimens, with less adverse effects and cheaper, is a major challenge for researchers.
Polyphenols
- Natural products containing high polyphenol levels as blackberries, red grapes, apricots, eggplant, coffee, cocoa, and green tea can regulate glucose metabolism through different paths, such as restoring beta-cell integrity, enhancing insulin-releasing activity, and increasing cellular glucose uptake, which can improve insulin resistance[rx].
Smart insulin patch
- A new smart insulin patch has been created. It is a thin square covered with more than 100 tiny needles. The patch made of biocompatible materials works fast and it’s easy to use. The patch consists of small painless needles that are packed together with insulin and glucose-sensitive enzymes in microscopic storage units. The patch releases these enzymes when blood glucose increases. In a mouse model, patch administration showed reduced glucose levels up to 9 h[rx]. It is suggested that the patch could have a longer effect in diabetic humans since humans are more sensitive to insulin than mice.
Dual-Acting Peptide
- GLP1 and GIP are the two main incretin hormones that are released from the intestine in response to food intake. Both hormones stimulate glucose-dependent insulin secretion. Evidence from animal studies suggests that anti-obesity efficacy of GLP1 can be enhanced by co-administration with the incretin hormone GIP. Finan et al[rx] showed that an acylated version of GLP1 and GIP dual agonist, reduced weight (-18.8% vs -8.8%, P < 0.001), food intake (P < 0.05), fat mass (P < 0.001) and blood glucose (P < 0.05), compared to liraglutide.
- Also showed increases in plasma insulin and C-peptide more pronounced that liraglutide (P < 0.001 for both). No differences in improved glycaemic control between these co-agonists and liraglutide were found. In T2DM patients they found a dose-dependent reduction of HbA1c, being -0.53% in patients treated with 4 mg of the dual agonist, and -1.11% in those treated with 30 mg, compared with placebo (-0.16%).
- The pharmacokinetics and pharmacodynamics results of co-activation of GLP1 and GIP receptors[rx] are considered as a promising new strategy for the treatment of obese T2DM patients, to prolong the activity of GLP1 and GIP dual agonists, and for the future development of a possible once-weekly GLP-1 and GIP dual agonists drug candidate for the treatment of T2DM.
GLP1 and Glucagon Receptor Dual Agonism
- Glucagon and GLP1 have distinct receptors that are also structurally related[rx]. Glucagon stimulates gluconeogenesis and glycogenolysis in the liver, raising blood glucose levels; while GLP1 reduce blood glucose levels by increasing insulin synthesis and secretion in the pancreas[rx]. Administration of oxyntomodulin, a GLP1 receptor/glucagon receptor dual agonist peptide, to rodents[rx–rx] and humans[rx,rx], resulted in an improvement of glucose metabolism by decreasing food intake and body weight and increasing energy expenditure, more pronounced than those reported by GLP1.
- Moreover, weekly administration of PEGylated peptides reduced adiposity and improved glucose tolerance in diet-induced obese mice[rx], and sustained GLP1/glucagon dual agonism reverses obesity in diet-induce obese mice[rx]. These co-agonist compounds also normalized glucagon, glucose and lipid metabolism and reduced liver steatosis, and is a novel therapeutic approach to the treatment of obesity in patients with T2DM.
GLP1 Receptor Agonist and Glucagon Receptor Antagonism Activity
- GLP1/Glucagon hybrid peptides, a dual acting peptide that binds both receptors, for diabetes (DAPD) have been reported previously[rx], and more recently have been identified in vitro[rx]. Administration of PEGylated DAPD in mice showed a decrease in blood glucose by increasing insulin secretion GLP1-induced, and a rise in fasting glucagon levels following a glucagon challenge[rx]. Moreover, unlike RA-GLP1, does not inhibit gastrointestinal motility and has not adverse events at this level.
Basal Insulin Analogs with Glucagon-Like Peptide-1 Mimetics
- The combination of GLP1 mimetics with basal insulin reduced the risk of hypoglycemia and weight gain induced for intensive insulin regimens in T2DM patients. Preliminary evidence suggests that the addition of basal insulin to a GLP1 mimetic with or without oral therapy, provide improvements in basal and postprandial glucose control, with less weight gain, reduced risk of hypoglycemia and increased satisfaction[rx–rx,rx–rx].
- Data from the DUAL I extension (insulin-naïve patients not controlled with oral hypoglycaemic agents) and DUAL II (patients not controlled on basal insulin plus oral hypoglycaemic agents) randomized trials, the novel fixed combination of insulin degludec and liraglutide (IDegLira), effectively lowered HbA1c across a range of measures, implying suitability for patients with either early or advanced T2DM[rx].
- LixiLan is a new once-daily single injection fixed-ratio combination of lixisenatide and insulin glargine. Results from the Lixilan-L trial showed that LixiLan successfully met the primary study endpoint of demonstrating a statistically superior reduction in HbA1c compared with insulin glargine[rx].
G Protein-Coupled Receptor 119
- G protein-coupled receptor 119 (GPR119) agonists is a G protein-coupled receptor that is expressed predominantly in the pancreas and gastrointestinal tract in rodents and humans, as well as in the brain in rodents[rx]. Activation of the receptor showed a reduction in food intake and body weight gain in rats[rx]. GPR119 has also been shown to regulate incretin and insulinsecretion[rx–rx]. New agents acting on this receptor have been suggested as novel treatments for obesity and diabetes[rx,rx].
- It is worth pointing out the potential advantages that could be obtained by the co-administration of a GPR119 agonist and an iDPP4. The role of these additional hormonal agents will require to clarify in the further study[rx].
Oral RA-GLP1
- Currently, RA-GLP1s are available only as injectables, either once daily or once weekly. Semaglutide is a long-acting RA-GLP1 that is also being developed as a once-weekly injectable. An oral semaglutide version leading to higher solubility and protection from enzymatic degradation is also being developed.
- The phase 2 study[rx] enrolled 632 adults with T2DM of 6 to 7 years duration, managed with lifestyle with or without metformin, and HbA1c 7.0% to 9.5% (mean, 7.9%). They were randomized to oral semaglutide in doses of 2.5, 5, 10, 20 or 40 mg once daily, or to placebo, or to open-label injected once-weekly 1.0-mg semaglutide. Patients started at 2.5 or 5 mg once daily and the higher-dose groups were titrated up at 4-wk intervals. The primary endpoint was changed in HbA1c from baseline to week 26.
- The proportion of patients achieving 5% or more weight loss was 21% to 71% in the oral group and 66% in the subcutaneous group, compared with 13% in the placebo group. None of the adverse events were considered serious and all were reported as mild to moderate in severity. Increases in lipase levels were greater in the oral and subcutaneous semaglutide groups, compared with placebo. Based on these data, oral semaglutide is now being studied in a large phase 3 trial[rx].
Oral insulin
- Oral administration of insulin is a novel treatment to improve glycaemic control in patients with T2DM. Oral insulin has a more physiological action than parenteral insulin. Due to its first pass through the liver, it reduces glycogenolysis, hepatic glucose production, and the risk of hypoglycemia, compared with parenteral insulin. Currently, the data available in human trials suggest that could be a novel approach to the treatment of diabetes[rx,rx].
Dual inhibition of SGLT1 and SGLT2
- Sotagliflozin is a dual inhibitor of SGLT1 and SGLT2 with approximately 20-fold selectivity for SGLT2 over SGLT1[rx]. Animal pharmacology studies showed that sotagliflozin produced increased urinary glucose excretion, delivery of glucose to the caecum, increased postprandial GLP1 and peptide YY release, that were related with significant reductions in postprandial glucose[rx,rx].
- Sotagliflozin was evaluated in patients with T2DM not controlled with metformin[rx]. Sotagliflozin reduced fasting plasma glucose and HbA1c with a modest urinary glucose excretion, compared with selective iSGLT2. The high glycaemic efficacy observed with only modest urinary glucose excretion suggested that clinically relevant gastrointestinal SGLT1 inhibition was present. Phase 1 and phase 2 studies have identified special opportunities for synergy with iDPP-4 for treatment of patients with T2DM and renal impairment.
Others
- Inhibitors of the sodium-glucose cotransporter 2, which increase renal glucose elimination, and inhibitors of 11ß-hydroxysteroid dehydrogenase 1, which reduce the glucocorticoid effects in liver and fat. Insulin-releasing glucokinase activators and pancreatic-G-protein-coupled fatty-acid-receptor agonists, glucagon-receptor antagonists, and metabolic inhibitors of hepatic glucose output are being assessed for the purpose of development of new drug therapy for type 2 diabetic patients.[rx]
Diet
- When nutritional intervention is contemplated, the co-morbidities that can coexist in a diabetic patient also have to be considered. The recommendations on dietary aspects can contribute to achieving the desired blood glucose, blood pressure, lipid profile and weight[rx,rx], as well as improve sleep apnoea, depression and quality of life related to health; in addition, it has been observed that the incidence of urinary incontinence in women is reduced[rx–rx].
- Numerous randomized controlled trials have demonstrated the metabolic benefits of nutritional recommendations in reducing HbA1c; being variables the results got depending mainly on the length of the disease[rx,rx].
Energetic Contribution
- Total caloric intake diet will depend on several factors, is determining the presence of overweight or obesity. Body mass index (BMI) is a tool commonly utilized in clinical practice to classify patients and it is calculated by the following equation: [weight (kg)/height (m2)]
[stextbox id=’info’]
Classification of the degree of obesity by body mass index
| Body mass index (kg/m2) | |
|
18.5-24.9 |
|
25-26.9 |
|
27-29.9 |
|
30-34.9 |
|
35-39.9 |
|
40-49.9 |
|
≥ 50 |
Adapted from World Health Organization (WHO) 1995, WHO 2000 and WHO 2004.
Different formulas for calculating baseline energy needs of people
| Harris-Benedict equation1 |
|
|
| Mifflin St Jeor equation2 |
|
|
[/stextbox]
Macronutrient Distribution
- There is not enough evidence to suggest an ideal percentage in the distribution of carbohydrates, lipids, and proteins. There are several studies that have sought to distribute the best ratio macronutrients without finding valid results and several dietary patterns that have been analyzed as the Mediterranean diet, vegetarian or vegan diet,
- Dietary Approaches to Stop Hypertension (DASH), low-fat diet and low carbohydrates diet observing modest effectiveness of managing diabetes. The benefits happen only when they are accompanied by a loose weight so more studies are needed[rx].
Carbohydrates
- Although there is no consensus on the percentage of carbohydrates that people with diabetes should eat, it has been shown that the amount and the type of carbohydrates are the main determinants for glycaemic control. Counting carbohydrates has proven to be very important in all patients.
- It allows a better adjustment of the postprandial blood glucose for those who take insulin. With this method, patients consumed a known amount of carbohydrates divided among different meals and calculated it in grams of carbohydrates per portion. This type of measurement is more important in patients with basal-bolus treatment or with continuous insulin infusion[rx].
[stextbox id=’custom’]
Glycaemic index, glycaemic load, and carbohydrates portion
|
|
amount of food containing 10 g of carbohydrates |
Glycaemic Research Institute. Available from: URL: http://www.glycemic.com/GlycemicIndex-LoadDefined.htm. GI: Glycaemic index.
[/stextbox]
- It is preferable that the intake of carbohydrates comes from products such as fruits, vegetables, legumes, whole grains and dairy vs those involve the added contribution of salt, fat or simple sugars[10].
Index and Glycaemic Load
- There is large confusion in the interpretation of the effect of the diet with low glycaemic index and there is not unanimity in the results of the different studies. Even though these diets are recommended by some associations because there are studies in which have been observed a better glycaemic control when it is compared above all with high glycaemic index food[rx], there are articles that have questioned this assertion.
- They based this divergence on The different definition of the glycaemic index, they do not take into account the fiber contribution and the different glycaemic response to the same food in different individuals. They consider that cannot be determinate that the observed effect is exclusively due to the food’s glycaemic load[rx]
Fiber
- Dietary fiber intake, especially the fiber that provides the natural resources, has shown that improve the control of cardiovascular risk factors, and improved the glycaemic control, turning into a lower risk of cardiovascular mortality in people with diabetes[rx,rx]. However, some studies have shown that the effect on diabetes has a modest significance and it is achieved with high amounts of fiber a day but this is far away from a real consumption in daily life (greater than 50 g/d)[rx].
- Generally, and taking into account the modest beneficial effects on cardiovascular risk factors, in diabetic patients is suggested a consumption of fiber and whole grains at least similar to that recommended for the general population; about 25 g/d for women, and 38 g/d for men or 14 g per 1000 kcal[rx].
Sucrose and Fructose
- Contrary to what one might think sucrose intakes of 10%-35% of total energy do not have a negative effect on glycaemic or lipid responses when sucrose is substituted for isocaloric amounts of starch[rx]. Consume free fructose (naturally occurring from foods such as fruit) did not get worsen the glycaemic control more than other forms of sugar, although it should avoid further intake of 12% of daily calories[rx].
- The restriction is advised of these sugars in the diet to avoid excessive caloric intake that can contribute to weight gain if are taken in large quantities. Moreover, sugary drinks contain large amounts of fast absorbing carbohydrates and have demonstrated a cardiovascular risk and diabetes increase in the healthy population that consumes them. Especially harmful when are sweetened with fructose free. Although there are not many studies on diabetic patients, there is no reason to think they will not have the same consequences. Therefore, the consumption of these drinks is contraindicated[rx].
Noncaloric sweeteners
- Opposite of natural simple sugars there are sweeteners with lower calorific value. Most are artificial. They do not have a caloric contribution, except aspartame (containing 4 kcal/g), and do not increase blood glucose. These sweeteners can be used by diabetic patients. If they are employed to replace glucose, bring the benefit of reducing the kilocalories in the diet[rx].
Proteins
- It is interesting to make a differentiation between diabetic patients with and without kidney disease. In people without kidney disease, protein intake usually recommended is between 15%-20%; however, reviewing scientific studies no firm conclusion could be reached with respect to this issue.
- In the literature, we can find different randomized clinical trials faced on this issue results. On the one hand there are studies that demonstrate that if 28%-40% of the energy of the diet is taken as proteins there is an improvement of the HbA1c, triglycerides, total cholesterol and/or LDL cholesterol[rx], while others studies have not shown a benefit in any of these aspects[rx].
- In patients with kidney disease, whether if we refer to micro or macroalbuminuria, reducing protein intake below the usual has been undergone various tests and meta-analysis and the evidence has not shown that improve glycaemic control, cardiovascular risk factors or renal disease progression following low-protein diets[rx]. With regard to the origin of proteins, there is no difference between animal and vegetable origin in relation to proteinuria[rx].
Fat
- Epidemiological studies have related fats with the risk of developing obesity and cardiovascular risk[rx]. As in the rest of immediate principles there is no optimal fat proportion and, as a general rule, the recommendations for the general population (between 20%-35%) are applied for a diabetic patient, paying special attention if the patient is overweight, then the percentage should be at the lower limits. Despite these recommendations, diabetic patients often take more fat than the recommended[rx].
- We can distinguish between saturated and unsaturated fats (monounsaturated and polyunsaturated). In addition, has to be specified that trans fatty acids may be a type of unsaturated fat but with harmful effects on the body for its different structure. Distinguish between these types is important because it has been demonstrated that quality is more relevant than the amount of fat consumed.
Omega-3 fatty acids
- Although there are unlike results, in general, we cannot say that omega-3 supplements have shown clear cardiovascular benefit[rx]. However, consumption of products high in omega-3 can be positive in preventing cardiovascular disease[rx].
Alcohol
- Alcohol should be drunk in moderation and it should not exceed one serving per day for women, or two servings per day in the case of men. To avoid an excess of energy when they are consumed, this contribution must be exchanged for other products. This moderate consumption does not harm the glycaemic control but rather in some studies has been found the contrary, with moderation can improve glycaemic control and reduce cardiovascular events.
- Despite the above facts, it is very important to note that alcoholic beverages may contribute to the appearance of late hypoglycemia especially in patients in treatment with hypoglycaemic drugs, so we should warn the patient to pay attention to any symptoms of hypoglycemia [rx].
Sodium
- The recommendation for the general population to reduce sodium intake to less than 2300 mg/d shall also apply to patients with diabetes mellitus. When these also have hypertension, which is very common, reduced sodium intake should be individualized[rx].
Specific Supplements
- The potential benefits of dietary supplements for diabetic patients with various specific nutrients have been subjected to trials. In spite of this, reliable data has not been observed to confirm benefits in glycaemic control supplementing because of supplement the diet with antioxidants as vitamin and carotenes, micronutrients such as chromium or other herbs. The recommendations of vitamins and minerals are not different from the general population, they are provided by a varied diet[rx].
Exercise
- The physical activity and exercise are one of the basic strategies in the treatment of diabetes. Promoting exercise, within a specific plan, provides in general terms multiple benefits: Increased insulin sensitivity in tissues, improvement of glycaemic control[rx], benefits in lipid profile and blood pressure, maintenance or weight loss, cardiovascular benefits, better quality of life, psychological well-being and improvement of depression[rx].
Benefits of glycaemic control
- In some studies, it has observed a significant decrease in HbA1c in patients with T2DM who do exercise. The difference in the degree of improvement observed in the different studies will depend on the characteristics of the patient and the type of training, thus, it is more effective when training programs are based on aerobic exercises of programs based on muscle strength in isolation[rx].
Other benefits
- The physical exercise also brings improvement in other metabolic parameters. It helps control cardiovascular risk factors (dyslipidemia, hypertension, weight maintenance, psychological benefits, reduces mortality, improvement cardiorespiratory fitness and peripheral neuropathy[rx,rx].
Types of Exercise
- Both aerobic and resistance exercises have demonstrated benefits in people with diabetes through increased glucose uptake and decreased insulin resistance. Though an aerobic exercise in isolation seems to get better benefits that resistance exercise[rx], in patients with diabetes is recommended the combination of both types because the effect is greater than if each one is performed in isolation[rx,rx].
- This type of training has been traditionally recommended for patients with T2DM. A frequency of at least 3 d per week is recommended, preferably if it can be increased to 5 d with no more than two consecutive days between periods of activity because the increase of the sensitivity and the glucose tolerance is maintained for about 12-24 h.
- It should be done with a moderate intensity which is 40%-60% of maximum aerobic capacity. Another method for measuring the intensity can be the subjective perception of the effort that assigns values to 20 points according to the patient judgment about the activity performed. A moderate-intensity exercise can also be an activity that can be conducted while maintaining an uninterrupted conversation.
Relationship between maximum oxygen consumption, % of maximum heart rate and subjective perceived exertion
[dropshadowbox align=”none” effect=”lifted-both” width=”auto” height=”” background_color=”#ffffff” border_width=”1″ border_color=”#dddddd” ]
| Intensity | % oxygen consumption | % maximum heart rate1 | Subjective perceived exertion |
|
< 20 | < 35 | < 10 |
|
20-39 | 35-54 | 10-11 |
|
40-59 | 55-69 | 12-13 |
|
60-84 | 70-89 | 14-16 |
|
> 85 | > 90 | 17-19 |
|
100 | 100 | 20 |
Unstructured Physical Activity
- It is also recommended to advise patients to increase energy expenditure in activities of daily life. It requires an increase of unstructured physical activity (walking more in the day, climb the stairs)[rx].
Prescription of a Specific Plan
- Exercise should be prescribed individually for each patient and taking into accounts the characteristics of the person. Initially, the guidelines should recommend a slow progression and, if it is necessary, the patient has to start with low volumes of work. Recommendations should take into account the type of diabetes and the treatment utilized, the possibility that patients have diabetic foot, retinopathy, neuropathy, nephropathy or some degree of cardiovascular risk[rx].
- Training plans that are supervised by professionals have proved to be more effective as this study has demonstrated. In it, is compared a supervised program against general advice, and although in both an increase in physical activity is observed, some better effects in HbA1c and cardiovascular risk factors in the supervised group have been seen[rx].
Exercise and Diabetes Complications
- The presence of diabetes complications involves a number of considerations at the time of writing prescriptions of physical exercise in these patients.
- The physical exercise has proved benefits in reducing the appearance of peripheral neuropathy[rx]. When it is already present, it is recommended to avoid exercises that cause impacts of repetition in the lower extremities and especially in patients with foot ulcers and wounds[rx]. Furthermore, recent studies have demonstrated that moderate intensity walking does not increase the risk of ulcers.
- The presence of retinopathy advises against the practice of physical activities that increase intrathoracic pressure (Valsalva maneuver), or high-intensity exercises by the risk of retinal detachment or intravitreal hemorrhage. The exercises with low and moderate intensity (walking, swimming…) are perfectly authorized and they can be done safely. Contact exercises like boxing should be avoided because of the risk of impact[rx].
- Exercise for diabetic patients is beneficial at any stage of renal function. In epidemiological studies, it has been shown to improve renal function. Promotes muscle strengthening in case of kidney failure that helps to counteract sarcopenia, and improves various parameters in patients on dialysis, so with supervision and restraint exercise is recommended and although they have been transient increases in microalbuminuria with sessions of exercise (because of increased blood pressure) is not considered as a marker of persistent microalbuminuria[rx].
- Physical activity has many beneficial cardiovascular effects but must take into account some considerations when there is a vascular disease. Patients with diabetes that present a moderate or high cardiovascular risk should be included in supervised cardiac rehabilitation programs, because exist an association with mortality. In addition, during the exercise, there is an increased activity of the sympathetic nervous system and catecholamines and decrease vagal tone[rx,rx].
- In people with peripheral arterial disease benefits from the practice of sports aerobics and resistance also exist because of the improvement of the mobility, functional capacity, pain tolerance and quality of life[rx].
- Moderate physical exercise can improve the autonomic nervous system both in patients with autonomic neuropathy and those who do not have it[rx], however it may represent a prescription limitation because it may favor silent ischemia, doubling mortality, impairing exercise tolerance and decreasing the maximum heart rate and thus a prior cardiovascular study is recommended[rx].
Exercise with Uncontrolled Blood Sugar
Hyperglycaemia
- In T2DM is very strange developing a true insulin deficiency, as in type 1 diabetic, so if the patient feels well is not necessary to postpone the exercise by hyperglycemia, although they must ensure an adequate hydration state[rx].
- In a non-diabetic person with aerobic exercise the increase of the glucose uptake is offset with a similar increase of the hepatic glucose, but in diabetic person, the muscle uptake is greater than the liver’s production although the risk of hypoglycemia is minimal if hypoglycaemic drugs are not taken[rx].
- However, if in addition to the effect of exercise add up the effects of hypoglycaemic drugs, we recommend a series of precautions mainly based on carbohydrate intake and adjust drug doses. If the levels before exercise are less than 100 mg/dL should take a supplement of 15 g of carbohydrates before exercise. This measure should only be recommended if blood glucose lowering drugs (secretagogues or insulin) are taken. If the control is with other drugs, supplements are not required if the exercise is less than an hour[rx]. It is important to note that regardless of the initial levels if the exercise is prolonged monitoring could be required and also intakes over the same period.
Complications
-
Neuropathy
-
Nephropathy
-
Retinopathy
-
Cardiomyopathy
-
Hypoglycemia
-
Diabetic ketoacidosis
-
Diabetic foot disease
-
Heart disease, heart attack, and stroke
-
Retinopathy and vision loss
-
Hearing loss
-
Foot damage such as infections and sores that don’t heal
-
Skin conditions such as bacterial and fungal infections
-
Depression
-
Dementia
Gestational diabetes
Uncontrolled gestational diabetes can lead to problems that affect both the mother and baby. Complications affecting the baby can include:
- premature birth
- higher-than-normal weight at birth
- increased risk for type 2 diabetes later in life
- low blood sugar
- jaundice
- stillbirth
References
[bg_collapse view=”button-orange” color=”#4a4949″ expand_text=”Show More” collapse_text=”Show Less” ]
- https://professional.diabetes.org/content/clinical-practice-recommendations
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2797383/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4478580/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3464757/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2613584/
- https://www.ncbi.nlm.nih.gov/books/NBK279119/
- https://www.ncbi.nlm.nih.gov/books/NBK513253/
- https://www.who.int/diabetes/en/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4673801/
- https://www.ncbi.nlm.nih.gov/books/NBK279509/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5027002/
- https://www.britannica.com/science/diabetes-mellitus
- https://my.clevelandclinic.org/health/diseases/7104-diabetes-mellitus-an-overview
[/bg_collapse]


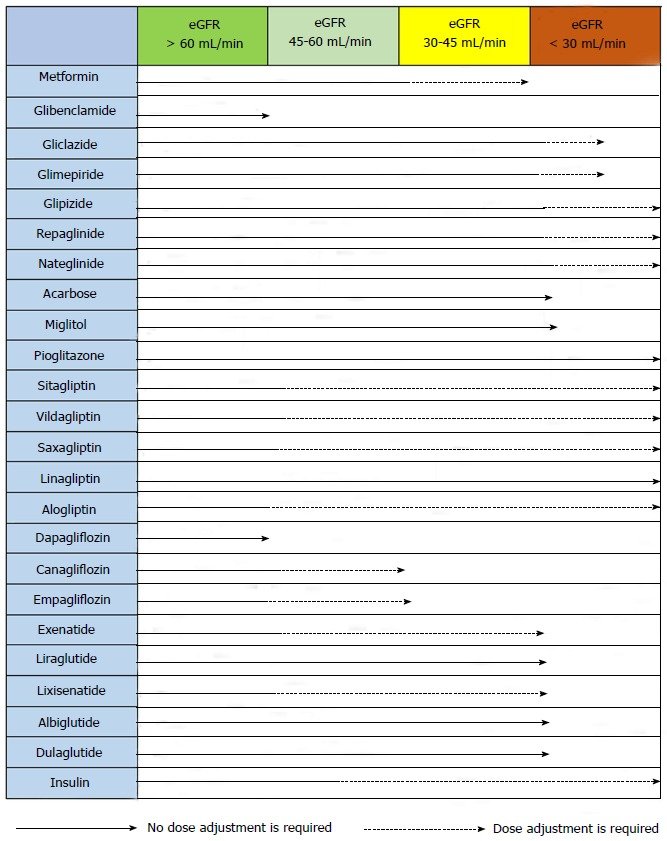
Visitor Rating: 5 Stars
Visitor Rating: 5 Stars
Visitor Rating: 5 Stars
Visitor Rating: 5 Stars