Bunion is a common deformity of the joint connecting the big toe to the foot. It is characterized by the first metatarsal bone deviating toward the midline of the body and the big toe deviating away from the midline of the body. This is often erroneously described as an enlargement of the metatarsal bone or tissue around the metatarsophalangeal joint. A similar condition of the little toe is referred to as a Tailor’s bunion or bunionette.
Hallux valgus is a deformity of the great toe, whereby the hallux (great toe) moves towards the second toe, overlying it in severe cases. This abduction (movement away from the midline of the body) is usually accompanied by some rotation of the toe so that the nail is facing the midline of the body (valgus rotation). With the deformity, the metatarsal head becomes more prominent, and the metatarsal is said to be in an adducted position as it moves towards the midline of the body. Radiological criteria for hallux valgus vary, but a commonly accepted criterion is to measure the angle formed between the metatarsal and the abducted hallux. This is called the metatarsophalangeal joint angle (also known as the hallux valgus angle, and hallux abducts angle), and it is considered abnormal when it is greater than 14.5°. A bunion is the lay term used to describe a prominent and often inflamed metatarsal head and overlying bursa. Symptoms include pain, limitation in walking, and problems with wearing normal shoes.
Epidemiology of adult Hallux Valgus
- More common in women
- 70% of pts with hallux valgus have family history & genetic predisposition with anatomic anomalies
Risk Factors
Intrinsic
- Genetic predisposition
- Increased distal metaphyseal articular angle (DMAA)
- Ligamentous laxity (1st tarsometatarsal joint instability)
- Convex metatarsal head
- 2nd toe deformity/amputation
- Pes planus
- Rheumatoid arthritis
- Cerebral palsy
Extrinsic
- shoes with high heel and narrow toe box
Anatomy of Hallux Valgus / Bunion
Effective treatment of hallux valgus depends on a solid understanding of the anatomy involved (see the images below).
- Lateral view of a first metatarsophalangeal joint with ligaments of the sesamoid complex.
- Plantar muscles that contribute to deforming forces.
- Valgus deviation of phalanx promotes the varus position of the metatarsal
- The metatarsal head displaces medially, leaving the sesamoid complex laterally translated relative to the metatarsal head
- Sesamoids remain within the respective head of the flexor hallucis Brevis tendon and are attached to the base of the proximal phalanx via the sesamoid-phalangeal ligament
- This lateral displacement can lead to transfer metatarsalgia due to the shift in weight bearing
- Medial MTP joint capsule becomes stretched and attenuated while the lateral capsule becomes contracted
- Adductor tendon becomes deforming force inserts on fibular sesamoid and lateral aspect of the proximal phalanx
- Lateral deviation of EHL further contributes to deformity
- Plantar and lateral migration of the abductor hallucis causes the muscle to plantarflex and pronate phalanx
- Windlass mechanism becomes less effective, leads to transfer metatarsalgia.
Associated conditions
- Hammertoe deformity
- Callosities
Juvenile and Adolescent Hallux valgus factors that differentiate juvenile/adolescent hallux valgus from adults
- Often bilateral and familial
- The pain usually not a primary complaint
- Varus of first MT with widened IMA usually present
- DMAA usually increased
- Often associated with flexible flatfoots
- Recurrence is a most common complication (>50%), also overcorrection and hallux varus
Risk factors /Causes of Hallux Valgus / Bunion
It is likely that the cause is multi-factorial. A number of risk factors have been noted to be associated with hallux valgus:
- Footwear – There is a significant association with wearing tight-fitting or high-heeled shoes. However, the condition can develop in people who have never worn such footwear and footwear is not usually a factor in juvenile hallux valgus. Equally not all people who wear high heels develop hallux valgus.
- Genetic predisposition.
- Gender – There is a higher incidence of hallux valgus in women. Footwear may account for this.
- Abnormalities of the foot – Pes planus (flat feet), Hypermobility, Achilles tendon contracture.
- Positional change due to neuromuscular conditions such as – Stroke, Cerebral palsy, Multiple sclerosis, Charcot-Marie-Tooth syndrome.
Systemic conditions causing ligament laxity
- Marfan’s syndrome.
- Ehlers-Danlos syndrome.
- Rheumatoid arthritis.
- Gout.
- Psoriatic arthropathy
Certain activities which may put greater force on the forefoot
- Ballet dancing – There is a weak association with ballet dancing. Dancers put a great deal of stress through the first MTP joint but it is unlikely that dancing causes bunions.
- Rock climbing
Symptoms of Hallux Valgus / Bunion
- Your big toe points toward your second toe or your second toe overlap your big toe
- A prominent bump on the inside of the MTP or big toe joint
- Pain on the inside of your foot at the big toe joint when wearing any kind of shoe
- Pain each time the big toe flexes when walking
- Redness, swelling, or thickening of the skin on the inside of the big toe joint
Indications for repair of hallux valgus include the following
-
Painful joint range of motion (ROM)
-
Deformity of the joint complex
-
Pain or difficulty with footwear
-
Inhibition of activity or lifestyle
-
Associated foot disorders that can be caused by this condition
Associated foot disorders include the following
-
Neuritis/nerve entrapment
-
The overlapping/underlapping second digit
-
Hammer digits
-
First, metatarsocuneiform joint exostosis
-
Sesamoiditis
-
Ulceration
-
Inflammatory conditions ( bursitis, tendinitis) of the first metatarsal head
Diagnosis of Hallux Valgus / Bunion
A bunion can be diagnosed and analyzed by plain projection radiography. The hallux valgus angle (HVA) is the angle between the longitudinal axes of the proximal phalanx and the first metatarsal bone of the big toe. It is considered abnormal if greater than 15-18°. The following HVA angles can also be used to grade the severity of hallux valgus.
- Mild: 15–20°
- Moderate: 21–39°
- Severe: ≥ 40°
The intermetatarsal angle (IMA) is the angle between the longitudinal axes of the first and second metatarsal bones and is normally less than 9°. The IMA angle can also grade the severity of hallux valgus as.
- Mild: 9–11°
- Moderate: 12–17°
- Severe: ≥ 18°
Physical exam
Hallux rests in valgus and pronated due to deforming forces illustrated above
Examine entire first ray for
- 1st MTP ROM
- 1st tarsometatarsal mobility
- callous formation
- sesamoid pain/arthritis
Evaluate associated deformities
- pes planus
- lesser toe deformities
- midfoot and hindfoot conditions
Radiographs
Views
- standard series should include weight-bearing AP, Lat, and oblique views
- the sesamoid view can be useful
Findings
- lateral displacement of sesamoids
- joint congruency and degenerative changes can be evaluated
- radiographic parameters (see below) guide treatment
Treatments of Hallux Valgus / Bunion
Non-surgical treatments
Non-surgical treatments for bunions may include
- Change your footwear! Relief from bunion pain can be as simple as changing the type of shoes you wear. Overall, wearing shoes that give the foot and toes ample room to move is the simplest way to prevent discomfort from bunions and are one of the most common bunion treatments. Ample space for the toes will prevent the big toe from being overcrowded, and ultimately pushing against the smaller toes.
Tips for proper shoe fit
- Size varies among brands, so be sure to judge the shoe by how it fits on your foot rather that the size marked on the shoe
- Find a shoe that is similar to the shape of your foot.
- Measure your feet regularly. The size of your feet tend to change as you grow older.
- Be sure to stand during the fitting process.
- Make sure you can extend all of your toes and that there is adequate space for your longest toe.
- Walk in the shoe to make sure it feels right.
- Shoes can also be stretched to relieve bunion discomfort. Bunion pads made from silicone can be used to line the area that presses against the bunion, relieving pain and preventing further deformity.
- If discomfort is still prevalent, consider visiting an orthopedist who can provide custom-made insole orthotics. Orthotics will ensure proper alignment of the foot and will reduce pressure on the bunion, making them very good among bunion treatments.
Taping your bunion – can also reduce the amount of pressure on the inflamed joint. Likewise, taping will help ensure that your foot is properly aligned. Consider visiting a medical professional or physical therapist to demonstrate the most beneficial and proper taping technique.
-
Anti-inflammatory Medication – Over-the-counter anti-inflammatory medications such as aspirin, ibuprofen, and naproxen can help to ease bunion inflammation and pain
-
Hot/Cold Bunion Therapy – Alternating ice and applying heat to a bunion can provide temporary pain relief caused by a bunion and may also help to reduce any swelling or bursitis in the big toe joint.
-
Castor Oil – Castor Oil is known as an anti-inflammatory and analgesic (pain relieving) holistic remedy and has been known to relieve the discomfort resulting from a bunion. Wrap a castor oil-soaked cloth around the foot ensuring the castor oil is in contact with the union. Then wrap the entire foot with plastic wrap. Finally, place a hot compress on the inflamed area for approximately 30 minutes.
-
Cortisone Injections –Inflammation of the joint at the base of the big toe and the pain associated with it can sometimes be relieved with a local injection of cortisone, a strong steroid used to reduce inflammation.
-
Acupuncture –This Chinese medical practice involving the insertion of needles at specified sites of the body has been shown to alleviate the pain caused by bunions.
-
Calcium & vitamin D3 – to improve bones health and healing fracture.
-
Glucosamine & diacerein– can be used to tightening the loose tension and regenerate cartilage or inhabit the further degeneration of cartilage.
- Corticosteroid – to healing the nerve inflammation and clotted blood in the joints.
- Dietary supplement – to remove the general weakness & improved the health. Using ice to provide relief from inflammation and pain. Using custom-made orthotic devices.
Surgery
Hallux valgus surgery: Specific goals
Eliminating acute pain and limited mobility due to hallux valgus
- Patients want to have anatomically normal, straight and cosmetically appealing feet after surgery, which are able to withstand the strain of sport and daily living.
Correction (osteotomy) of the phalanges
- The important correction aims at preventing wear (arthritis) in the metatarsophalangeal joint and problems in the forefoot (such as hammertoes and metatarsal pain). The goal is to permanently normalize the gait and the mechanics of roll-off whilst walking.
Stabilizing the metatarsophalangeal joints for arthritis
- The important metatarsophalangeal joint can suffer arthritis (joint wear) due to the hallux valgus deformity. This joint wear can either be treated by preserving the joint (arthroscopy) or fusing the joint (arthrodesis). There is also the option of the full or partial prosthesis (Hemi prosthesis) of the metatarsophalangeal joints.
The principle of hallux valgus surgery
- There are now many different hallux valgus surgery techniques. Before looking more closely at the important procedures in a different article on → hallux surgery, we would like to quickly single out the principles of correcting hallux valgus they all have in common. All specific procedures on the metatarsophalangeal joint include these treatment options.
Soft tissue procedures: Treating the tendons and joint capsule of the big toe
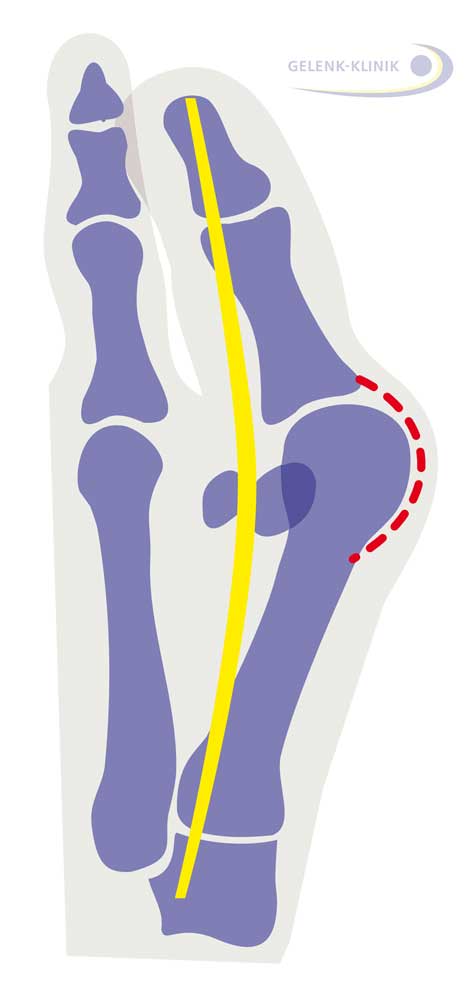
- The tendon of the big toe is shown in yellow. It strains the big toe like a bow. Shown in red is the joint capsule, increasingly strained in hallux valgus.
- The capsule around the metatarsophalangeal joint has narrowed due to the deformity so the deformity is contrakt, i.e. can no longer be actively returned. So the release and expansion of the joint capsule and adjusting the length of the tendons controlling the big toe is an important step in achieving permanent straightening of the big toe.
- The joint capsule changes due to hallux valgus. On the side of the bend in the metatarsophalangeal joint (red in the adjacent drawing) the capsule is overstretched, on the other side, it is contracted. This change to the joint capsule must be corrected through condensation and expansion. The affected tendons (yellow) also require length correction.
Osteotomy: Repositioning the bones and healing in the new position
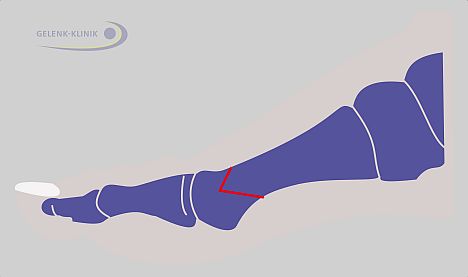
- Osteotomy (bone repositioning) – The direction of the foot ray can be changed permanently with a cut to the bone (red line) and realignment. Once healed, the change of direction can permanently correct hallux valgus. The chevron osteotomy shown here is one of many repositioning options which can be used based on the individual case.
- With surgical osteotomy – the metatarsus and phalanges are severed and joined again in a new, desired direction, and stabilized with screws, wire or small metal splints until healed into place in the new position.
Cheilectomy: Joint-preserving arthroscopy of the metatarsophalangeal joint
- If the joint is still more than 50% cartilage, a joint-preserving, minimally invasive arthroscopy of the metatarsophalangeal joint can be performed. Any bone spurs which are present are removed. The prospects of cheilectomy must sometimes be determined during surgery, after having a direct view of the joint. If the damage is already too severe, this procedure cannot provide any relief for problems.
Arthrodesis: Fixation of the metatarsophalangeal joint
- In patients with severe hallux valgus deformity and arthritis of the metatarsophalangeal joint sometimes the big toe must be removed entirely and fixed. This fixation is done by fusing the joint partners. If necessary, this fusion (especially in women) has an angle which also allows for wearing higher heels without restricting motion.
“Minimally invasive” surgical technique with minimal incisions and minimal scarring
- Medical advancements have developed many different hallux valgus surgical methods.
- The most promising hallux valgus surgical technique was developed in recent years. It is internationally proven but so far only performed by a small number of Germany clinics: The so-called minimally invasive hallux valgus surgery. By using tiny instruments only 2mm large, similar to dental instruments, injury to the soft tissue during the hallux surgery, and hence the healing time, can be considerably reduced.
Special Characteristics: With this hallux valgus surgery, no screws are installed for minor deformities. This eliminates the need for follow-up surgery to remove the screws.
[stextbox id=’custom’]
A selection of well-known surgical procedures for the treatment of hallux valgus
| Name | Site | Advantages/disadvantages | Comments | |||
| Akin | Proximal phalanx | In combination with other techniques, stability technically difficult | Used in hallux valgus interphalangeal | |||
| Metatarsophalangeal joint arthrodesis | Metatarsophalangeal joint | Permanent correction, loss of mobility, subsequent osteoarthritis | Used in severe deformities and/or hallux rigidus | |||
| Basal osteotomy | Metatarsal I, proximal | In combination with soft tissue intervention, stability technically difficult, implant necessary, not possible if the tarsometatarsal joint is unstable | Suitable for correction of severe deformities | |||
| Chevron | The reliable technique, little soft tissue trauma, implant necessary, not possible with severe deformity, reduced perfusion of the head of the metatarsal I | Used in mild deformities | ||||
| Hohmann | Metatarsal I, distal | Little stability with wires or sutures, reduced perfusion of the head of metatarsal I | Now hardly ever used | |||
| Hueter | Simple technique, lack of support for the head of metatarsal I, transfer metatarsalgia frequent | No longer used | ||||
| Keller-Brandes | Proximal phalanx, proximally | Simple technique, loss of hallux function, transfer metatarsalgia frequent | Used in elderly and inactive patients | |||
| Kramer | Metatarsal I, distal | Little stability with wires, reduced perfusion of the head of metatarsal I | Now hardly ever used | |||
| Lapidus | Tarsometatarsal joint | In combination with soft tissue intervention, implant necessary, loss of mobility, technically difficult, the danger of pseudarthroses | Used in cases of TMT-I joint instability or osteoarthritis | |||
| Metatarsophalangeal joint | Frequent recurrence owing to the inadequate correction of metatarsal I | Now hardly ever used, replaced by soft tissue procedure | ||||
| Scarf | Metatarsal I, diaphyseal | Accurate correction angle, implant necessary, extensive soft tissue dissection | Suitable for correction of mild to moderate deformities | |||
| Soft tissue procedure | Metatarsophalangeal joint | Complete soft tissue correction, two skin incisions necessary | Usually in combination with a proximal osteotomy |
| Comparison | Results | Comments | ||
| Chevron osteotomy versus Wilson osteotomy | Quicker return to work with Chevron osteotomy, a better functional outcome with Wilson osteotomy | Three years’ follow-up, Wilson osteotomy now hardly ever used | ||
| Chevron osteotomy with versus without adductor tenotomy | Hallux correction 9.8°/7.5° with/without tenotomy, no other differences | Limited relevance, because capsule not divided | ||
| Rehabilitation with versus without continuous motion after Chevron osteotomy | Mobility better with continuous motion | Only 90 days’ follow-up, limited relevance for treatment | ||
| Curved versus proximal Chevron osteotomy | No significant differences regarding correction, but swifter and more reliable healing with proximal Chevron osteotomy | Only 2 years’ follow-up, various fixation techniques, limited relevance for treatment | ||
| Suture versus screw fixation in Mitchell osteotomy | Better results with screws | Superior stability with screws was to be expected, Mitchell osteotomy now seldom used | ||
| Surgery versus 1-year conservative treatment with or without orthesis | Surgery superior to conservative treatment after 1 year, no difference after 2 years | Unclear interpretation of data | ||
| Hohmann osteotomy versus Lapidus operation | No significant difference, also not with regard to hypermobility of first tarsometatarsal joint | No severe deformities included only 2 years’ follow-up | ||
| Lindgren versus Chevron osteotomy | No significant differences, both procedures suitable only for mild deformities | Long follow-up (6 years); comparison of two very similar techniques; Lindgren techniques now seldom used | ||
| Scarf osteotomy versus Chevron osteotomy | No significant differences, good results in both groups | Comparison of two very similar techniques; the authors recommend Chevron osteotomy because it is technically simpler | ||
| Screw versus K-wires for stabilization; curved, distal metatarsal osteotomy | No significant differences, good results in both groups | Groups too small, limited relevance for treatment | ||
| Exercises versus night splint in conservative hallux valgus treatment | No difference between the groups | Groups too small | ||
| Chevron osteotomy with fixation (resorbable peg) versus no fixation, with plaster versus elastic bandage postoperatively | Osteotomy displacement 3.9 mm with fixation versus 3.1 mm without fixation (statistically significant), no difference for postoperative treatment | Accuracy of measurement technique not described, difference clinically irrelevant |
[/stextbox]
Physical Therapy Management
As a result of the gait disturbances (see non-operative treatment), objectives for physical therapy could be:
- Adjusted footwear with the wider and deeper tip
- Increase extension of MTP joint
- Sesamoid Mobilization: Relieve weight-bearing stresses (orthosis)
- The physical therapist performs grade III joint mobilizations on the medial and lateral sesamoid of the affected first MPJ. One thumb is placed on the proximal aspect of the sesamoid and is used to apply a force from proximal to distal that causes the sesamoid to reach the end range of motion (distal glides). These are performed with large-amplitude rhythmic oscillations. No greater than 20° of movement of the MPJ should be allowed during the technique.
- Strengthening of peroneus longus
Gait Training
- Stance phase: could be trained by performing a heel-strike in its physiological position at the lateral aspect of the heel.
- Stance phase could be followed by weight-bearing of the first metatarsal during midstance and terminal stance, with the training of active push-off by the hallux flexors, the flexor digitorum longus and brevis muscles and the lumbrical muscles
During gait training, verbal cues could be provided.
These objectives should ensure that pain is reduced and function is restored.
Physiotherapists should contain an expanded program, including whirlpool, ultrasound, ice, electrical stimulation, MTJ mobilizations, and exercises. This is more effective than physical therapy alone. The combination will result in an increase in ROM of the MTP joint, strength and function, and also a decrease in pain.
PHASE I – Pain Relief. Minimize Swelling & Injury Protection
- Pain is the main reason that patients seek treatment for a bunion. Inflammation is best eased using ice therapy, techniques (e.g. soft tissue massage, acupuncture, unloading taping techniques) or exercises that unload the inflamed structures. Anti-inflammatory medications may help. Orthotics can also be used to offload the bunion.
PHASE II – Restoring Normal ROM & Posture
- As pain and inflammation settle, the focus of treatment turns to restore normal toe and foot joint range of motion and muscle length.
Treatment may include;
- joint mobilization (abduction and flexion) and alignment techniques (between the first and the second metatarsal)
- massage
- muscle and joint stretches
- taping
- bunion splint or orthotic
- bunion stretch and soft tissue release.
PHASE III – Restore Normal Muscle Control & Strength
- A foot posture correction Program to assist you to regain your normal foot posture.
Dorsiflexion Strengthening with Elastic Resistance Band
- The ankle dorsiflexion exercise strengthens the ankle and lower leg muscles. The patient is positioned in long sitting. The center of the resistance band is placed on the top of the forefoot with the toes slightly pointed. The ends of the band are either held by an assistant or secured against an immovable object (e.g. a table leg). The patient then dorsiflexes the ankle, pulling “towards their nose,” working against the resistance of the band.
Towel curls
- The patient spreads out a small towel on the floor, curling his/her toes around it and pulling the towel towards them.
Toes spread out (TSO)
- A possible causative factor of the hallux valgus is the muscle imbalance between the abductor hallucis and the adductor hallucis. Strengthening the abductor’s muscle can prevent a hallux valgus and can be helpful to correct the deformity in an early stage. The toes-spread-out (TSO) exercise is an efficient way to train abductor hallucis.
PHASE IV – Restoring Full Function
- The goal of this stage of rehabilitation is to return the patient to his/her desired activities. Everyone has different demands for their feet that will determine what specific treatment goals need to be achieved.
PHASE V – Preventing a Recurrence
- Bunions will deform further with no attention and bunion-associated pain has a tendency to return. The main reason is biomechanical. In addition to muscle control, the physiotherapist should assess foot biomechanics and may recommend either a temporary off-the-shelf orthotic or refer for a custom-made orthotic. High heeled shoes and shoes with tight or angular toe boxes should be avoided.
Complications of surgery
These may depend on the procedure but can include:
- Delayed healing of the incision,
- Osseous malunion or non-union,
- Nerve damage,
- Hematoma,
- Failure of a prosthesis,
- Displacement of the osteotomy,
- Delayed suture reaction,
- Cellulitis,
- Osteomyelitis,
- Avascular necrosis,
- Limitation of joint motion,
- Hallux varus,
- Recurrence,
- Risks associated with all surgery, especially if the patient is elderly. This includes venous thromboembolism.
References
[bg_collapse view=”button-orange” color=”#4a4949″ expand_text=”Show More” collapse_text=”Show Less” ]
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3528062/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3528062/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5467633/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4668189/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4004226/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2955707/
[/bg_collapse]

Visitor Rating: 5 Stars