Chronic Neck Pain/ Cervical spondylosis is a chronic degenerative condition of the cervical spine that affects the vertebral bodies and intervertebral discs of the neck (in the form of, for example, disk herniation and spur formation), as well as the contents of the spinal canal (nerve roots and/or spinal cord). Some authors also include the degenerative changes in the facet joints, longitudinal ligaments, and ligament flavum.
Cervical spondylosis is a common progressive degenerative disorder of the human spine often caused by the natural aging process. It is defined as “vertebral osteophytosis secondary to degenerative disc disease” due to the osteophyte formations that occur with progressive spinal segment degeneration [rx–rx]. Early spondylosis is associated with degenerative changes within the intervertebral disc where desiccation of the disc occurs, thus causing overall disc height loss and a reduction in the ability of the disc to maintain or bear additional axial loads along the cervical spine [rx, rx]. At birth, the intervertebral discs are healthy, with the proteoglycan matrix within the nucleus pulposus maintaining a 70% to 90% water content which declines with aging [rx]. As the water content declines within the nucleus pulposus, the once healthy glistening gelatinous appearance changes into a darkened and discolored fibrous “crabmeat” consistency with a loss in water content and a loss in the structural integrity.
Alternative Name
Cervical osteoarthritis; Arthritis – neck; Neck arthritis; Chronic neck pain; Degenerative disk disease, degenerative disc disease, cervical spondylotic myelopathy, cervical spine stenosis
Pathophysiology & Etiology

Degenerative cervical spondylosis (CSM)
- The most common cause of cervical myelopathy
- Compression usually caused by anterior degenerative changes (osteophytes, disc osteophyte complex)
- Degenerative spondylolisthesis and hypertrophy of ligamentum flavum may contribute
Congenital stenosis
- Symptoms usually begin when congenital narrowing combined with spondylotic degenerative changes in older patients
- OPLL
- Tumor
- Epidural abscess
- Trauma
- Cervical kyphosis
Neurologic injury
Mechanism of injury can be
- direct cord compression
- ischemic injury secondary to compression of the anterior spinal artery
Associated conditions
- Lumbar spinal stenosis tandem stenosis occurs in the lumbar and cervical spine in ~20% of patients
- Prognosis natural history tends to be slowly progressive and rarely improves with nonoperative modalities
- progression characterized by steplike deterioration with periods of stable symptoms
- prognosis early recognition and treatment prior to spinal cord damage is critical for good clinical outcomes
Causes of Chronic Neck Pain
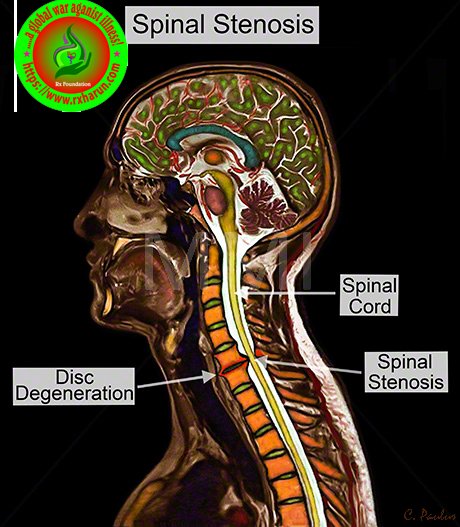
- Bone spurs – Sometimes, an overgrowth of bone can occur as the body is trying to grow extra bone to help make the spine stronger. The extra bone can push against the spinal cord and nerves.
- Dehydrated discs – Gel-like material inside the discs between bones can dry out over time. This causes bones to rub together. This drying out typically begins around age 40.
- Herniated discs – Spinal discs can develop cracks, which allow cushion material to leak and press on the spinal cord and nerves.
- Injury – A fall, a car accident, or any injury to the neck can speed up aging.
- Ligament stiffness – Cords connecting the spinal bones can become stiff over time and make it difficult to move the neck.
- Overuse – Early wear and tear can occur if someone’s occupation or hobbies involve repetitive movements or heavy lifting.
Major and severe causes of neck pain (roughly in order of severity) include
- Carotid artery dissection
- Referred pain from acute coronary syndrome
- Head and neck cancer
- Infections: retropharyngeal abscess, epiglottitis, etc.
- Spinal disc herniation – protruding or bulging discs, or if severe prolapse.
- Spondylosis – degenerative arthritis and osteophytes
- Spinal stenosis – a narrowing of the spinal canal
The more common and lesser neck pain causes include
- Stress – physical and emotional stresses
- Prolonged postures – many people fall asleep on sofas and chairs and wake up with sore necks.
- Minor injuries and falls – car accidents, sporting events and day to day injuries that are really minor.
- Referred pain – mostly from upper back problems
- Over-use – muscular strain is one of the most common causes
- Whiplash
- Herniated disc
- Pinched nerve
Symptoms of Chronic Neck Pain
-
Cervical pain aggravated by movement
-
Referred pain (occiput, between the shoulder blades, upper limbs)
-
Retro-orbital or temporal pain (from C1 to C2)
-
Cervical stiffness—reversible or irreversible
-
Vague numbness, tingling, or weakness in upper limbs
-
Dizziness or vertigo
-
Poor balance
-
Rarely, syncope triggers a migraine, “pseudo-angina
-
Poorly localized tenderness
-
Limited range of movement (forward flexion, backward extension, lateral flexion, and rotation to both sides)
-
Minor neurological changes like inverted supinator jerks (unless complicated by myelopathy or radiculopathy)

- Neck stiffness and pain >axial neck pain (often times absent) & occipital headache common
- extremity paresthesias >diffuse nondermatomal numbness and tingling
- A headache that may originate in the neck
- Pain in the shoulder or arms
- Inability to fully turn the head or bend the neck, sometimes interfering with driving
- Grinding noise or sensation when the neck is turned
- Tingling, numbness, and/or weakness in the arms, hands, legs, or feet
- Lack of coordination and difficulty walking
- Abnormal reflexes
- Muscle spasms
- Loss of control over bladder and bowel (incontinence
- weakness and clumsiness
- weakness and decreased manual dexterity (dropping object, difficulty manipulating fine objects)
- gait instability
- the patient feels “unstable” on feet
- weakness walking up and down stairs
- gait changes are a most important clinical predictor
- urinary retention rare and only appear late in disease progression not very useful in diagnosis due to high prevalence of urinary conditions in this patient population motor.
“Red flag” features and the conditions they may suggest
Malignancy, infection, or inflammation
-
Fever, night sweats
-
Unexpected weight loss
-
History of inflammatory arthritis, malignancy, infection, tuberculosis, HIV infection, drug dependency, or immunosuppression
-
Excruciating pain
-
Intractable night pain
-
Cervical lymphadenopathy
-
Exquisite tenderness over a vertebral body
Myelopathy
-
Gait disturbance or clumsy hands, or both
-
Objective neurological deficit—upper motor neuron signs in the legs and lower motor neuron signs in the arms
-
Sudden onset in a young patient suggests disc prolapse
Other
-
History of severe osteoporosis
-
History of neck surgery
-
Drop attacks, especially when moving the neck, suggest vascular disease
-
Intractable or increasing pain
Diagnosis of Chronic Neck Pain
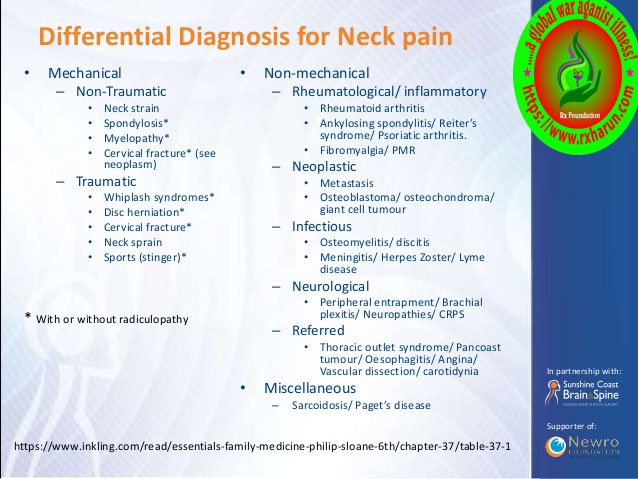
Differential diagnosis of Chronic Neck Pain
-
Other non-specific neck pain lesions—acute neck strain, postural neck ache, or whiplash
-
Fibromyalgia and psychogenic neck pain
-
Mechanical lesions—disc prolapse or diffuse idiopathic skeletal hyperostosis
-
Inflammatory disease—rheumatoid arthritis, ankylosing spondylitis, or polymyalgia rheumatica
-
Metabolic diseases—Paget’s disease, osteoporosis, gout, or pseudo-gout
-
Infections—osteomyelitis or tuberculosis
-
Malignancy—primary tumors, secondary deposits, or myeloma
Common Clinical Presentation and Examination Tools
Motor signs
-
Weakness in triceps and hand intrinsics
-
Atrophy of intrinsic hand muscles
-
Clumsiness with fine motor skills
-
Proximal weakness of the lower extremities
Upper motor neuron signs
-
Hoffman’s sign (quick flexion of both the thumb and index finger when the middle finger nail is snapped)
-
Inverted radial reflex (flexion of the fingers in response to the brachioradialis reflex)
-
Pathological clonus
-
Babinski sign
Sensory dysfunction
-
Glove-like sensory loss in hands
-
Proprioceptive dysfunction
Assessment tools
-
Lhermitte sign
-
Romberg test
-
9-Hole peg test
-
Grip and release test (observe decrease number of cycles)
-
Timed gait, 30-m walking test
-
Tandem gait
-
Triangle step test
The key parameters are osteophyte formation, intervertebral disc height narrowing, and vertebral end-plate sclerosis.
grade 0 (normal)
- no degenerative changes
Grade 1 (minimal/early)
- minimal anterior osteophyte formation
- no reduction of intervertebral disc height
- no vertebral endplate sclerosis
Grade 2 (mild)
- definite anterior osteophyte formation
- subtle or no reduction in Intervertebral disc height (<25%)
- just recognisable sclerosis of the endplates
Grade 3 (moderate)
- definite anterior osteophyte formation
- moderate narrowing of the disc space (25-75%)
- definite sclerosis of the endplates and osteophyte sclerosis
Grade 4 (gross)
- large and multiple large osteophyte formation is seen
- severe narrowing of the disc space (>75%)
- sclerosis of the endplates with irregularities
Physical exam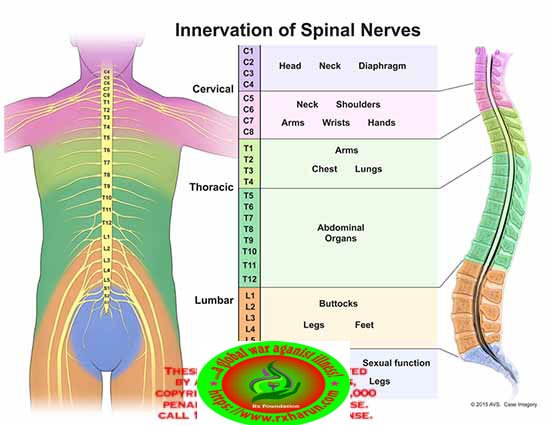
Motor
Weakness
- usually difficult to detect on physical exam
- lower extremity weakness is a more concerning finding
- when patient holds fingers extended and adducted, the small finger spontaneously abducts due to weakness of intrinsic muscle
Grip and release test
- normally a patient can make a fist and release 20 times in 10 seconds. myelopathic patients may struggle to do this
- sensory
Proprioception dysfunction
Grip and release test
Normally a patient can make a fist and release 20 times in 10 seconds. myelopathic patients may struggle to do this sensory, proprioception dysfunction
Decreased pain sensation
- pinprick testing should be done to look for a global decrease in sensation or dermatomal changes
- due to the involvement of lateral spinothalamic tract
Vibratory changes are usually only found in the severe case of long-standing myelopathy with upper motor neuron signs (spasticity)
Hyperreflexia
- may be absent when there is concomitant peripheral nerve disease (cervical or lumbar nerve root compression, spinal stenosis, diabetes)
Inverted radial reflex
- tapping distal brachioradialis tendon produces ipsilateral finger flexion
- snapping patients distal phalanx of middle finger leads to spontaneous flexion of other fingers
- > three beats defined as sustained clonus
- sustained clonus has poor sensitivity (~13%) but high specificity (~100%) for cervical myelopathy
- considered positive with the extension of the great toe
Gait and balance
- toe-to-heel walk patient has difficulty performing
- the patient stands with arms held forward and eyes closed
- loss of balance consistent with posterior column dysfunction
Provocative tests
- Lhermitte Sign >test is positive when extreme cervical flexion leads to electric shock-like sensations that radiate down the spine and into the extremities
Radiographs
Recommended views
- cervical AP, lateral, oblique, flexion, and extension views
General Findings
- Degenerative changes of uncovertebral and facet joints
- Osteophyte formation
- Disc space narrowing
- Decreased sagittal diameter – cord compression occurs with canal diameter is < 13mm
- Lateral radiograph – important to look for the diameter of spinal canal a Pavlov ratio of less than 0.8 suggest a congenitally narrow spinal canal predisposing to stenosis and cord compression sagittal alignment C2 to C7 alignment, determined by tangential lines on the posterior edge of the C2 and C7 body on lateral radiographs in neutral position local kyphosis angle
the angle between the lines drawn at the posterior margin of most cranial and caudal vertebral bodies forming the maximum local kyphosis - Oblique radiograph – important to look for foraminal stenosis which often caused by uncovertebral joint arthrosis
- Flexion and extension views – important to look for angular or translational instability & look for compensatory subluxation above or below the spondylotic/stiff segment
- Sensitivity/specificity – changes often do not correlate with symptoms 70% of patients by 70 yrs of age will have degenerative changes seen on plain x-rays
Modified Japanese Orthopaedic Association Scoring System.[rx]
| Motor dysfunction | |
| Upper extremities | |
| 0 | Unable to move hands |
| 1 | Unable to eat with a spoon but able to move hands |
| 2 | Unable to button shirt but able to eat with a spoon |
| 3 | Able to button shirt with great difficulty |
| 4 | Able to button shirt with slight difficulty |
| Lower extremities | |
| 0 | Complete loss of motor & sensory function |
| 1 | Sensory preservation without the ability to move legs |
| 2 | Able to move legs but unable to walk |
| 3 | Able to walk on the flat floor with a walking aid (cane or crutch) |
| 4 | Able to walk up- &/or downstairs w/aid of a handrail |
| 5 | Moderate-to-significant lack of stability but able to walk up &/or downstairs without a handrail |
| 6 | Mild lack of stability but able to walk unaided with smooth reciprocation |
| 7 | No dysfunction |
| Sensory dysfunction | |
| Upper extremities | |
| 0 | Complete loss of hand sensation |
| 1 | Severe sensory loss or pain |
| 2 | Mild sensory loss |
| 3 | No sensory loss |
| Sphincter dysfunction | |
| 0 | Unable to micturate voluntarily |
| 1 | Marked difficulty in micturition |
| 2 | Mild-to-moderate difficulty in micturition |
| 3 | Normal micturition |
MRI
MRI is a study of choice to evaluate the degree of the spinal cord and nerve root compression
- effacement of CSF indicates functional stenosis
- spinal cord signal changes are seen as a bright signal on T2 images (myelomalacia)
signal changes on T1-weighted images correlate with a poorer prognosis following surgical decompression - compression ratio of < 0.4 carries poor prognosis CR = smallest AP diameter of cord / largest transverse diameter of cord
Sensitivity/specificity
- has high rate of false positive (28% greater than 40 will have findings of HNP or foraminal stenosis)
CT without contrast
- can provide complementary information with an MRI, and is more useful to evaluate OPLL and osteophytes
CT myelography
- more invasive than an MRI but gives excellent information regarding degrees of spinal cord compression
- useful in patients that cannot have an MRI (pacemaker), or have an artifact (local hardware)
- contrast is given via C1-C2 puncture and allowed to diffuse caudally, or given via a lumbar puncture and allowed to diffuse proximally by putting the patient in Trendelenburg position.
Nerve conduction studies
- high false negative rate
- may be useful to distinguish peripheral from the central process (ALS)
Electromyogram (EMG) – This test measures the electrical activity in your nerves as they send signals to your muscles when the muscles are contracting and when they’re at rest. The purpose of an EMG is to assess the health of your muscles and the nerves that control them.
- Nerve conduction study. For this test, electrodes are attached to your skin above the nerve to be studied. A small shock is transmitted through the nerve to assess the strength and speed of nerve signals.
- Alar ligament and Transverse ligament test– test for instability of the upper cervical spine.
- Spurling sign – used to look for radicular comparable pain when the neck is in extension and lateral flexion toward the lesion(foraminal encroachment). Specificity is 92%for neurologic and radiological signs.
- Lhermitte sign – used to look for the comparable sign in neck extension.
- Hoffman sign – looks for a reflex contraction of the thumb and index finger occurs in response to nipping of the middle finger. This sign is evidence of an upper motor neuron lesion. A Hoffman sign may be insignificant if present bilaterally.
Treatment of Chronic Neck Pain
Non- Pharmacological
- Cold and Heat – Applying a cold pack to the painful part of the back contracts inflamed muscle and relieves pain. This treatment helps a great deal when the disk has recently ruptured and swelling is at its greatest. A heating pad or warm pack helps with residual pain.
- Continued Physical Activity – Though pain or weakness seem like good reasons to rest the neck, excessive bed-rest worsens the symptoms of a slipped disc in neck. Moving around too little allows muscles to grow weaker and prevents the body from healing. Periods of rest interspersed with periods of normal activity throughout the day keep the back muscles in shape.
- Physical Therapy – Physical therapists show slipped disc sufferers ways to move that do not cause pain. Occupational therapists teach skills that allow patients to return to a productive life.
- Nutrition – In order to restore the disc we also are going to need to include different substances in our diet. There are a lot of supplements on the market, of course. If you wish to try them, that’s fine. I personally don’t like them. I have tried one with glucosamine and chondroitin, but I didn’t feel any different. So, if you have the opportunity to take these with the food or from more natural sources, it will be great. You can find these substances in seafood and animal cartilages and by digesting them we ensure the building blocks for the connecting tissue for our joints and spine. Also, we will need more
- Omega 3 fatty acids – which can be supplied from cold pressed oils, fatty fish, flax seeds, chia and many more. Vitamins from the B group are very beneficial for people with herniated discs and all kinds of issues with the peripheral nervous system. Vitamins B1, B6 and B12 nourish the nerves and help them recover from the disk accident. Usually, doctors prescribe them as a part of the treatment, but it is worth mentioning anyway.
- A good massage – A massage is one of the natural methods of relieving pain. Individuals who get a massage weekly for several months stand a better chance of alleviating neck pain. A good massage provides a person with many health benefits that lessen neck pain. A massage triggers the release of endorphins. Endorphins aid in decreasing anxiety and relieving pain. They offer a relaxation effect by softening muscles that are injured preventing cramping.
- Undertaking yoga – Yoga is an applicable strategy for keeping the level of back pain at minimal levels. Taking yoga sessions often is very an effective method of dealing with neck pain. With yoga, there is a high likelihood of proper body functions. The use of pain prescriptions is also diminished. Patients suffering from neck pain related issues do not have to rely on these prescriptions to manage pain. Incorporating laughter in yoga is a good way of exercising. Yoga incorporates simple yet appropriate exercises that enhance the stretching of muscles. Laughter with yoga stimulates relieving of pain. It facilitates increased uptake of oxygen, little anxiety, and production of endorphins. All these variables play an essential role in diminishing neck pain.
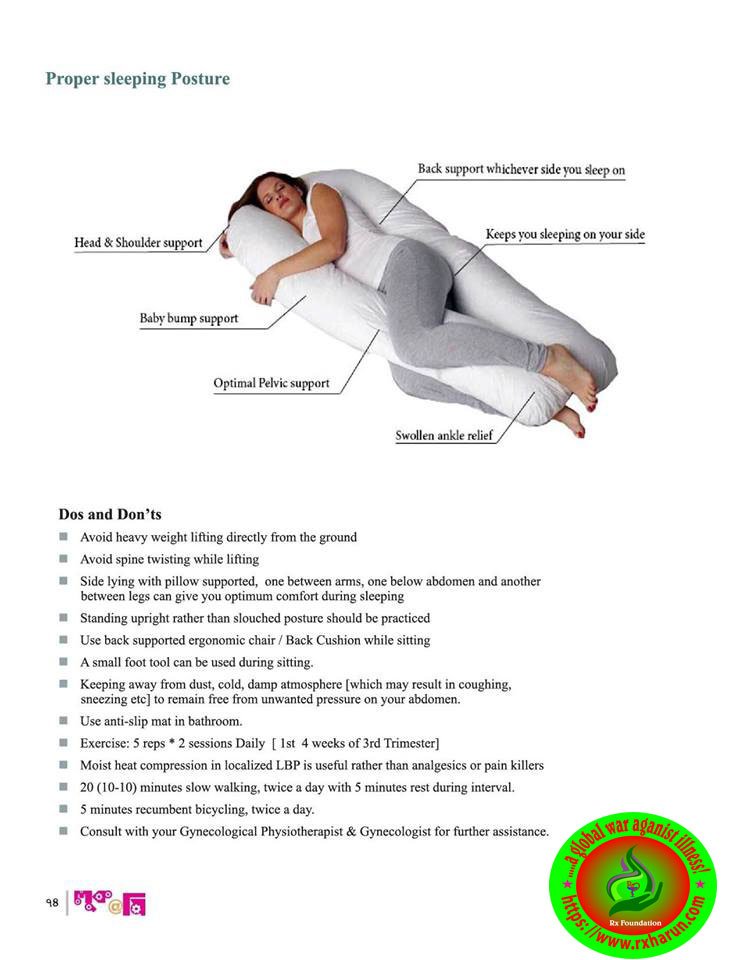
- Adjusting sleeping position – A simple sleeping mistake can immensely contribute to neck pain. A poor sleeping position can cause stress and tension on the muscles contributing to neck pain. Altering one’s sleeping position and adopting a style that does not exert a lot of stress on the back is a recommended tactic. Nurturing sleeping habits such as assuming a reclining position, using wedge-shaped cushions and getting adjustable beds from reputable medical institutions are easy techniques to endorse. If a reclining position does not suit an individual, the other two techniques can be embraced.
- Heat therapy – Several considerations should be observed when using heat therapy. The right temperature ought to be set so as to ensure a patient does not face risks associated with too much exposure to heat. The key objective should be to ensure enough access to heat to the muscles to yield benefits for the patient. The adoption of heat therapy for easing neck pain is determined by the magnitude of pain a person is experiencing. In cases where relatively low back pain is encountered, short heat therapy sessions are recommended. On the other hand, if an individual is experiencing prolonged back pain, long heat therapy sessions are the most applicable.
- Taking hot baths – This is a form of heat therapy that aims at relieving neck pain. It guarantees permeation of heat into the muscles leading to reduced pain. Many individuals opt for this method since they believe it achieves competent results. Hot baths initiate a fast process of blood supply to stiff neck muscles. When this happens, the muscles relax and stretch leading to decreased pain. To avoid interference with one’s sleeping patterns, a hot bath should be taken several hours before retiring to bed.
- Aquatic therapy – This natural technique involves physical therapy in a pool. Individuals get the best out of this therapy by relying on the resistance of water. Consistency in undertaking this therapy is what ascertains getting back pain relief. Integrating aquatic therapy in an individual’s life for the better part of the week enhances the reduction of back pain quickly.
- Enlighten others – Individuals have the power to devise their own natural strategies that aid them in coping with back pain. The strategies can also be a good remedy for others going through similar circumstances. An individual can use social media platforms to equip others with important tips on how to keep back pain at bay. Further, becoming a member of associations that address back pain issues enables better communication of the knowledge gained from personal experience.
Medications
Consultation with a health care provider is advised before use. The following are the main types of medications used for low back pain:
- Analgesic medications – are those specifically designed to relieve pain. They include OTC acetaminophen and aspirin, as well as prescription opioids such as codeine, oxycodone, hydrocodone, and morphine. Opioids should be used only for a short period of time and under a physician’s supervision. People can develop a tolerance to opioids and require increasingly higher dosages to achieve the same effect. Opioids can also be addictive. Their side effects can include drowsiness, constipation, decreased reaction time, and impaired judgment. Some specialists are concerned that chronic use of opioids is detrimental to people with back pain because they can aggravate depression, leading to a worsening of the pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDS) – relieve pain and inflammation and include OTC formulations (ibuprofen, ketoprofen, and naproxen sodium). Several others, including a type of NSAID called COX-2 inhibitors, are available only by prescription. Long-term use of NSAIDs has been associated with stomach irritation, ulcers, heartburn, diarrhea, fluid retention, and in rare cases, kidney dysfunction and cardiovascular disease. The longer a person uses NSAIDs the more likely they are to develop side effects. Many other drugs cannot be taken at the same time a person is treated with NSAIDs because they alter the way the body processes or eliminates other medications.
- Anticonvulsants—drugs primarily used to treat seizures—may be useful in treating people with radiculopathy and radicular pain.
- Antidepressants – such as tricyclics and serotonin and norepinephrine reuptake inhibitors have been commonly prescribed for chronic low back pain, but their benefit for nonspecific low back pain is unproven, according to a review of studies assessing their benefit.
- Muscle Relaxants – If the muscles around the slipped disc experience painful spasms, a muscle relaxant such as Valium may be useful. The drawback to drugs like these is that they do not limit their power to the affected nerve. Instead, they have a generally relaxing effect and will interfere with daily activities. Such as cyclobenzaprine (Flexeril), might be prescribed to relieve the discomfort associated with muscle spasms. However, these medicines might cause confusion in older people. Depending on the level of pain, prescription pain medicines might be used in the initial period of treatment.
- Steroids – If inflammation is severe, a doctor may also prescribe a steroid. Steroids, such as cortisone, reduce swelling quickly. A cortisone shot directly in the affected area will have an immediate effect on the displaced disc.
- Counter-irritants – such as creams or sprays applied topically stimulate the nerves in the skin to provide feelings of warmth or cold in order to dull the sensation of pain. Topical analgesics reduce inflammation and stimulate blood flow.
- Nerve Relaxant — Pregabalin or gabapentin and anti-inflammatory drugs help to relieve pain and stiffness, allowing for increased mobility and exercise. There are many common over-the-counter medicines called non-steroidal anti-inflammatory drugs (NSAIDs). They include aspirin, ibuprofen (Motrin, Advil), and naproxen (Naprosyn, Aleve).
- Spinal manipulation and spinal mobilization – Are approaches in which professionally licensed specialists (doctors of chiropractic care) use their hands to mobilize, adjust, massage, or stimulate the spine and the surrounding tissues. Manipulation involves a rapid movement over which the individual has no control; mobilization involves slower adjustment movements. The techniques have been shown to provide small to moderate short-term benefits in people with chronic low neck pain. Evidence supporting their use for acute or subacute low neck pain is generally of low quality. Neither technique is appropriate when a person has an underlying medical cause for neck pain such as osteoporosis, spinal cord compression, or arthritis.
- Traction – Involves the use of weights and pulleys to apply constant or intermittent force to gradually “pull” the skeletal structure into better alignment. Some people experience pain relief while in traction, but that relief is usually temporary. Once traction is released the back pain tends to return. There is no evidence that traction provides any long-term benefits for people with low back pain.
- Spinal injections — An injection of a cortisone-like anti-inflammatory medicine into the lower back might help reduce swelling and inflammation of the nerve roots, allowing for increased mobility.
- Nerve block therapies – Aim to relieve chronic pain by blocking nerve conduction from specific areas of the body. Nerve block approaches range from injections of local anesthetics, botulinum toxin, or steroids into affected soft tissues or joints to more complex nerve root blocks and spinal cord stimulation. When extreme pain is involved, low doses of drugs may be administered by catheter directly into the spinal cord. The success of a nerve block approach depends on the ability of a practitioner to locate and inject precisely the correct nerve. Chronic use of steroid injections may lead to increased functional impairment.
Treatment for symptoms due to cervical spondylosis aims to relieve pain and prevent permanent damage to your nerves.
- Over-the-counter painkillers
- Non-steroidal anti-inflammatory drugs (NSAIDs) are thought to be the most effective painkillers for symptoms due to cervical spondylosis. Some commonly used NSAIDs include
- diclofenac
- ibuprofen
- aceclofenac
- naproxen
- pentadol
- However, NSAIDs may not be suitable if you have asthma, high blood pressure, liver disease, heart disease or a history of stomach ulcers. In these circumstances, paracetamol would probably be more suitable. Your pharmacist or GP will be able to advise you.
- Codeine – If your pain is more severe, your GP may prescribe the mild opiate painkiller called codeine. This is often taken in combination with NSAIDs or paracetamol. A common side effect of taking codeine is constipation. To prevent constipation, drink plenty of water and eat foods high in fiber, such as wholegrain bread, brown rice, pasta, oats, beans, peas, lentils, grains, seeds, fruit, and vegetables.
- Amitriptyline – If pain persists for more than a month, and has not responded to the above painkillers, your GP may prescribe a medicine called amitriptyline. Amitriptyline was originally designed to treat depression, but doctors have found that a small dose is also useful in treating nerve pain. You may experience some side effects when taking amitriptyline. They include:
- drowsiness
- dry mouth
- blurred vision
- constipation
- difficulty urinating
Do not drive if you find that amitriptyline is making you drowsy. Amitriptyline should not be taken by people with a history of heart disease.
- Gabapentin – Gabapentin (or a similar medication called pregabalin) may also be prescribed by your GP for helping radiating arm pain or pins and needles caused by nerve root irritation. This medicine is otherwise used as an anti-epileptic drug. Some people may experience side effects that disappear when they stop the medication, such as a skin rash or unsteadiness. Gabapentin needs to be taken regularly for at least two weeks before any benefit is judged.
- Injection of a painkiller – If your radiating arm pain is particularly severe and not settling, there may be an option of a ‘transforaminal nerve root injection’, where steroid medication is injected into the neck where the nerves exit the spine. This may temporarily decrease inflammation of the problem nerve root and reduce pain.
- Soft cervical collar – This is a padded ring that wraps around the neck and is held in place with velcro. Your doctor may advise you to wear a soft cervical collar to limit neck motion and allow the muscles in your neck to rest. A soft collar should only be worn for a short period of time since long-term wear may decrease the strength of the muscles in your neck.
- Ice, heat, and other modalities – Your doctor may recommend careful use of ice, heat, massage, and other local therapies to help relieve symptoms.
- Steroid-based injections – Many patients find short-term pain relief from steroid injections. The most common procedures for neck pain include:
- Cervical epidural block – In this procedure, steroid and anesthetic medicine is injected into space next to the covering of the spinal cord (“epidural” space). This procedure is typically used for neck and/or arm pain that may be due to a cervical disk herniation, also known as radiculopathy or a “pinched nerve.”
- Biofeedback – It is used to treat many acute pain problems, most notably back pain and headache. The therapy involves the attachment of electrodes to the skin and the use of an electromyography machine that allows people to become aware of and self-regulate their breathing, muscle tension, heart rate, and skin temperature. People regulate their response to pain by using relaxation techniques. Biofeedback is often used in combination with other treatment methods, generally without side effects. The evidence is lacking that biofeedback provides a clear benefit for low back pain.
Physiotherapy Management in Chronic Neck Pain

Physiotherapy is usually the first non-surgical treatment that your doctor might recommend. Specific exercises can help relieve pain, strengthen and stretch the muscles weakened or strained. In some cases, physiotherapy may include posture therapy or the use of traction to stretch the joints and muscles of your neck gently. Physiotherapy programs vary in length but usually last for 6-8 weeks. Typically, sessions are scheduled 2 to 3 times a week.
- Medial branch block and radiofrequency ablation – This procedure is usually done for some chronic neck pain It can be used for both diagnosis and treatment of a potentially painful joint.
- Cervical facet joint block – In this procedure, steroid and anesthetic medicine is injected into the capsule of the facet joint. The facet joints are situated at the back of the neck and stability and movement. Arthritis may be formed and will play a part to neck pain.
- The patient is advised to use the cervical collar in case of the cervical spine and lumbar corset in the lumbar spine.
- Bed rest.
- Static cervical and lumbar exercises.
- Intermittent mechanical traction for 20 minutes daily.
- Moist/heat therapy can relieve pain and muscle spasm.
- SWD, US, MWD etc. to relieve chronic inflammation and pain.
- Interferential therapy in cases of acute conditions.
- Transcutaneous electrical nerve stimulator (TENS) can be given to relieve radicular pains.
- Gentle mobilization techniques can be used to regain range of motion and to relieve stiffness.
- Electrical stimulation – TENS unit may be issued to a patient for home use. E-stimulator is used to stimulate your muscles through variable intensities of electrical current. It helps to decrease muscle spasms and also act as a natural painkiller. TENS also drive out inflammation, herald healing properties, relax and re-educate the muscles which involved.
- Heat therapy – Physiotherapist uses different healing modalities to improve blood circulation to the target area because an increased blood flow brings more O2 and nutrients to that area. Blood is also needed to remove waste created by muscle spasms, and it also assists in decrease pain.
- Soft tissue manipulation – This technique targets spasms and chronic muscle tension and pain that perhaps build up through daily life stress. You could also have spasms or muscle tension because of strains or sprains.
Home Remedies For Chronic Neck Pain

- Use Cow’s ghee in your food. It is the best natural “Vata” reliever and gives nourishment to the nerves and other body parts.
- A tablespoonful of Turmeric should be consumed once every day, after boiling it in milk for half an hour. It is a very useful herbal treatment for cervical spondylosis.
- Constipation must be avoided at all costs. Constipation may increase pain in cervical spondylosis.
- Herbs have divine healing powers and they have the ability to cure any disease of the root. They were gifted to us by God when he created life. So believe in God if you want to get rid of your problems!
- Ayurvedic herbs are unique natural remedies for cervical spondylosis. Ayurvedic principles are different in many ways from modern medicine for example – Drinking water from a copper pan after keeping it overnight is also very useful in rheumatoid arthritis and cervical spondylosis.
- Consuming castor oil at night with milk or alone is a very useful herbal remedy for arthritis, especially rheumatoid arthritis and cervical spondylosis.
- Improve your nutrition as the first step. It plays an important role to fight diseases. When nothing works, nutrition works a lot!
- Use herbal juices like Aloe vera juice (Kumari Saar) and Amla Juice (Amla Saar) in routine. Amla is the richest source of natural Vitamin C. Vitamin C improves the natural immunity of the body. 100 gm of Amla juice contains 30 times more vitamin C than 100 gm of oranges.
Homeopathy for Chronic Neck Pain

- Shallaki (Boswellia serrata) – Boswellia serrata is a very popular natural anti-inflammatory herb used by Ayurveda physicians all over the world. It is commonly known in India as ‘Salai Guggul’. The resin obtained from the tree is purified and then used for pain and inflammation. It relieves cervical Spondylosis and other arthritis pains naturally without causing any side effects.
- Guggul (Commiphora Mukul) – Commiphora Mukul is a known anti-inflammatory agent used by Ayurveda physicians worldwide. The analgesic and anti-inflammatory action is almost immediate. Guggul is also used in weight loss formulas and is effective in reducing weight, thus it also helps osteoarthritis patients as well as cervical Spondylosis pains.
- South (Zingiber officinale) – It is commonly known as dry ginger. Dry Ginger is another useful anti-inflammatory herb. It also improves appetite and good for the digestive and respiratory system and helps to control data element.
- Ashwagandha (Withania somnifera) – Ashwagandha is popularly known as Indian ginseng in the west. It has known anti-inflammatory, anti-cancer, and anti-stress activities.
- Ashwagandha (Withania somnifera) – The herb also possesses anti-inflammatory, antitumor, antistress, antioxidant, immunomodulatory, hemopoietic, and rejuvenating properties. It is especially useful in diabetics and blood pressure people as it also controls diabetes and blood pressure. It relieves stress, anxiety and enhances physical and mental performance naturally.
- Tagar (Valeriana wallichii) – It is commonly known as ‘Valerian’ and is a very popular herb in the west. It is used in India for its benefits in calming down the nervous system. It relieves stress and anxiety and also fights depression. It also relaxes muscles and is very useful among natural herbal remedies for Cervical Spondylosis.
- Brahmi (Bacopa monnieri) – The herb ‘Brahmi’ is used in Ayurveda since ages for loss in memory, lack of concentration, forgetfulness. It increases the retention power as well as recollection. It is very useful in many mental illnesses also. Regular use also helps in stress, anxiety, blood pressure, hallucinations, and epilepsy. Regular use of this herb improves mental ability and cognition.
Dos and Don’ts of Handling Chronic Neck Pain
- Avoid Acid-Forming Foods – Foods that make your body more acidic increase your body’s rate of inflammation and keep you from healing as fast as you would like. Sugar, fried food, refined flour, alcohol, and tobacco should all be avoided as much possible or at least limited if you wish to manage the pain that comes with cervical spondylosis
- Sunlight – Sunlight in moderation is good for anything that ails you. It lightens your mood and releases feel-good endorphins in your body which makes it easier to handle any uncomfortable muscle pains.
- Work on Your Posture – A lifetime of slouching and bad posture will cause your spinal cord to grow in incorrect angles which cause the vertebrae to push against each other. By standing tall, you stretch out your spinal cord and give the vertebrae a chance to set correctly.
- Wear a Neck Brace – If the neck ache is both chronic and severe, where even small movements result in waves of pain, then invest in a neck brace. The brace will help support your neck and let the muscles heal unimpeded.
- Sleep on Your Back – Lying flat down at night without a pillow will allow your spine to set into its natural position.
- Don’t Overexert Yourself – Your spinal cord will be especially prone to serious injuries if you have this condition. Therefore, you should avoid very strenuous exercise to prevent further damage.
- Massages – Regular massaging can loosen the stiff vertebra in your neck allowing for less painful and freer movement
References
[bg_collapse view=”button-orange” color=”#4a4949″ expand_text=”Show More” collapse_text=”Show Less” ]
- https://www.ncbi.nlm.nih.gov/pubmed/17204889
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1819511/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3116771/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1307540/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5582708/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4264061/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3287027/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4716725/
[/bg_collapse]

Visitor Rating: 5 Stars