Osteoarthritis Spine Anatomy Causes Exercise is known as degenerative of spinal joints, the breakdown of the cartilage, tendon, ligaments of the joints and discs in the neck and lower back. Sometimes, osteoarthritis produces spurs that put pressure on the nerves leaving the spinal column. This can cause weakness and pain in the arms or legs.
Types of Arthritis
However, inflammation is typically absent in osteoarthritis until the later stages of the disease. Because of this, osteoarthritis can go by several different names including:
- Spondylosis
- Osteoarthrosis
- Spinal Stenosis
- Degenerative Joint Disease
- Degenerative Disc Disease
The joints are the connection between two bones that allow movement while providing support. In between the bones of the joint is a cavity filled with liquid known as synovial fluid.
Covering the ends of each bone is a type of flexible, yet strong, connective tissue known as articular cartilage. The synovial fluid acts as a shock absorber and helps to prevent wear and tear of this cartilage caused by friction. The cartilage further protects the bones from everyday wear and tear and also helps to absorb shock.
Our spine, or vertebral column, is set up a bit differently than other joints. The spine is broken down into five different sections:
- The Neck, or Cervical Spine
- Mid-back, or Thoracic Spine
- Lower back, or Lumbar Spine
- Upper portion of the pelvic cavity, or Sacral Spine
- Tailbone, or Coccyx
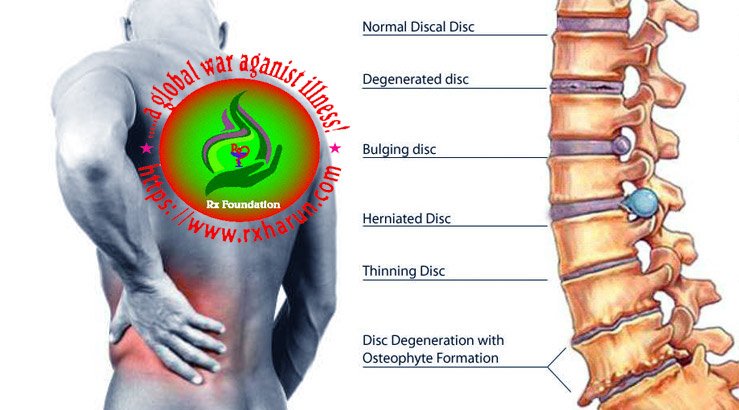
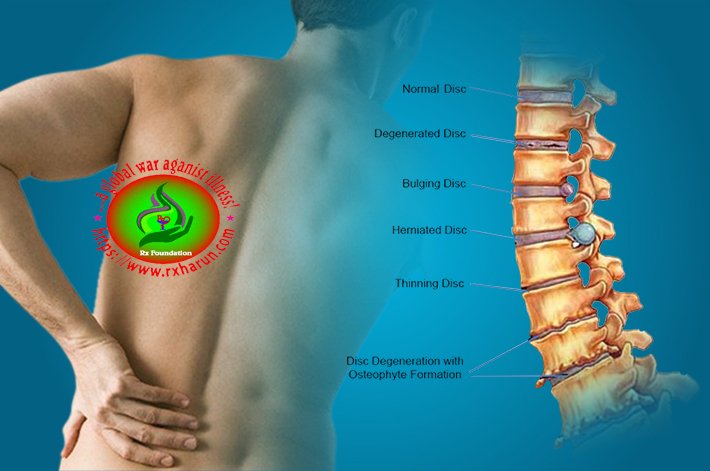
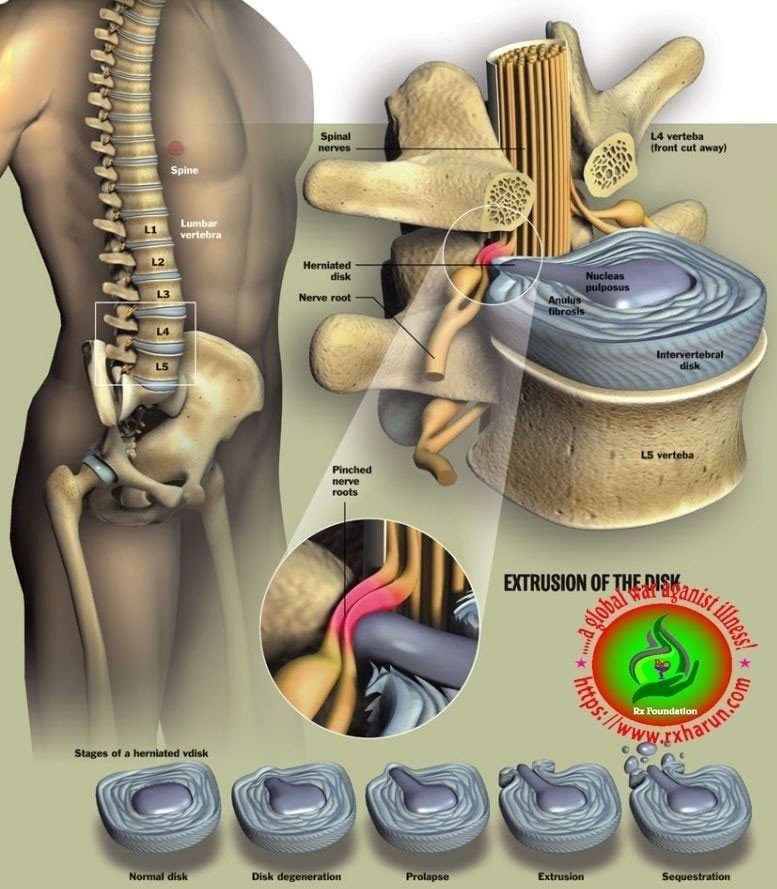
It has 24 individual vertebrae (essentially the joints) and is covered in cartilage as well. However, the spine has gel-like pads, called discs, instead of cavities filled with synovial fluid.
These discs are filled with a fluid that is comprised of degenerated collagen, proteoglycans and water. This gel-like center is called the nucleus pulposus, and it acts as the shock absorber for the spine.
- Age
Genetic factors
- Heritability estimates for hand, knee and hip OA are about 40-60%.
- The responsible genes are largely unknown.
Local, largely biomechanical risk factors
- Joint injury.
- Occupational and recreational stresses on joints.
- Reduced muscle strength.
- Joint Laxity.
- Joint malalignment.
Constitutional factors
- Aging.
- Female sex.
- Obesity.
- High bone density – a risk factor for the development of OA.
- Low bone density – a risk factor for progression of knee and hip OA
- Weight – “Carrying around excess weight increases the wear and tear on your spine,” notes Dr. Kovacs.
- Back injury – A history of trauma to your spine or a history of spinal surgery can increase your risk of developing spinal arthritis. Additionally, joint injury is a common cause of osteoarthritis in younger populations, according to NIAMS.
- Stress and strain – Repetitive strain on the neck and back from leaning, twisting, and lifting can also increase the risk of osteoarthritis. This may be from athletic activities like hockey, football, gymnastics, or weightlifting, as well as from certain occupations.
- Spinal misalignment – Scoliosis, a sideways curvature of the spine, or other forms of spinal misalignment can put stress on the joints and increase the risk of spinal osteoarthritis.
- Family history – Osteoarthritis tends to run in families, according to the University of Maryland Medical Center in Baltimore. And specific genes are associated with a higher risk of other types of arthritis, including rheumatoid arthritis and ankylosing spondylitis, according to the Centers for Disease Control and Prevention.
New Guidelines
In 2012, the American College of Rheumatology (ACR) released updated recommendations for drug and non-drug treatment of hand, knee, and hip osteoarthritis. Key points include:
- The recommendations emphasize the early use of non-drug treatments, especially aerobic, aquatic, and resistance exercise. Overweight patients are encouraged to lose weight. While not strongly recommended, the ACR considers tai chi, acupuncture, and transcutaneous electrical stimulation (TENS) appropriate options for some patients.
- For patients older than 75 years old, the ACR recommends skin-applied (topical) NSAIDs instead of oral NSAIDs. For older patients, topical NSAIDs pose less risks for stomach bleeding and other side effects. (However, see Drug Warning below.)
- Topical capsaicin, a pain reliever derived from chili pepper, is recommended for hand osteoarthritis but not knee or hip osteoarthritis.
- The ACR does not recommend the use of glucosamine and chondroitin supplements.
Symptoms of Osteoarthritis of Spine
Osteoarthritis causes the breakdown of the articular cartilage and primarily affects the weight bearing joints including the knees, hips and spine. However, it can affect any of the joints such as the fingers and toes.
As the articular cartilage degenerates, the bones begin to rub against each other causing friction. Over time, this friction causes the bones to become worn down essentially compressing the joint. In the later stages, this can cause inflammation, which exacerbates the problem and the pain.
Osteophytes, or bone spurs, begin to grow on the bones where the articular cartilage is worn down. This is Mother Nature’s attempt at healing the degeneration.
Unfortunately, bone spurs can lead to even more problems including interfering with the blood flow to the vertebrae and the curvature of the spine. This can cause stiffness in the joints and a very uncomfortable feeling called “locking.”
Locking is essentially a joint getting stuck. It can be very painful, or there may be no pain whatsoever. It can be very disconcerting, but normally the joint will unlock with a little bit of gentle manipulation. Osteophytes can also cause entrapment of the spinal nerves, and spinal stenosis (loss of space for the nerves to pass through).
Osteoarthritis is one of the leading causes of back pain, and the pain it causes in the joints is difficult to distinguish from muscle pain. When osteoarthritis settles into the spine, the vertebrae aren’t the only parts affected. The discs are affected as well.
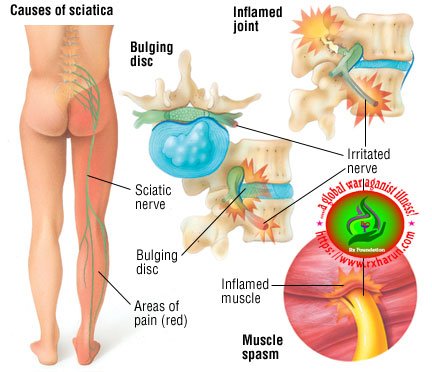
Degeneration of the vertebral joints causes excessive strain on the discs, which can cause dehydration of the nucleus pulposus (the gel-like center) of the disc. As a result, the ability to absorb shock and lubricate the joint is lost. This can lead to a number of problems including:
- Bulging of the disc out of the vertebral space
- Compression of the vertebrae
- Herniation in which the jelly-like contents escape through a thinned portion of the disc wall and spill into the spinal canal, which can put pressure on the spinal nerves
Symptoms of spinal osteoarthritis can be very similar to other forms of arthritis. Some of these symptoms include:
- Stiffness in the neck or back, particularly the lower back
- Weakness, numbness or tingling of the legs and arms
- Migraines (caused by compression of the cervical vertebrae)
- Constant pain in the neck, or back that is only relieved by laying down
- Problems performing routine tasks and hobbies
- Psychological effects caused by chronic pain
according to the web MD page
- Pain, tenderness or numbness in the neck
- Low back pain that extends into the buttocks, thighs or hips
- Pain or tenderness in the shoulders, hips, knees or heels
- A “crunching” sensation, or the sound of bone against bone
- Weakness or numbness in the legs or arms
- Limited range of mobility, difficulty bending or walking
- Spinal deformity
Symptoms are typically worse in the morning and evening, and on humid, rainy or cold days.
Barometric pressure and weather changes (such as a change from warm to cool air) can exacerbate symptoms.
Because we sleep for 8 hours or more in the supine or similar position, osteoarthritis symptoms are typically the worst upon waking and for the first 30 minutes after rising.
Joints affected by the disease become stiff after long periods in a single position such as sitting or sleeping, and this stiffness can be very painful.

Crepitus, or cracking sounds, can occur after being in one position for long periods. The sound is caused by the bones of the joints rubbing together, or a bone spur rubbing against one of the bones of the joint. Crepitus tends to occur more frequently in the neck, hips, and knees.
Many people with osteoarthritis notice improvement in their pain after exercising. I’m one of these people. Cardio exercise and weight training exercises have made a huge difference in my pain levels.
Causes of Osteoarthritis of Spine
Lower back pain is mainly triggered due to the condition of osteoarthritis of the lumbar spine. Due to this degenerative joint diseases, the lumbar joints become inflamed which results in severe pain, restricted mobility and in extreme cases it may result in permanent paralysis. If you are experiencing the following cases it is of utmost importance that you consult your doctor immediately.
Degeneration or wear and tear of the joints due to the natural process of aging.
- Injury or trauma, such as a car accident that triggers the process of joint cartilage erosion or joint irritation.
- Repetitive stress injury like typing on the computer for long hours without taking a break or lifting heavy load on a daily basis is one of the most common causes of osteoarthritis.
- The hereditary cause may also contribute to osteoarthritis.
- Disc degeneration may also cause osteoarthritis. The intervertebral disc supporting the two lumbar vertebra may undergo degeneration due to stress and aging. This may cause pain, stiffness and difficulty in moving the lumbar joint.
- The exercise-induced injury is most common among active individuals like athletes. This is because the increased activity level increases friction when the bones in the joints rub against each other. This causes wearing off of the cartilage and the supporting structures that provide joint stability.
- Wear and tear due to aging Injuries such as whiplash
- A genetic cartilage defect
- Poor posture
- Repetitive movement
- Obesity
- Poor diet
- Genetics
- Gender
- Other diseases such as diabetes or gout
Lab Diagnostic of Osteoarthritis of Spine
Laboratory tests and x-rays are often used in addition to these criteria.
Osteoarthritis of the hand can often be diagnosed on the basis of these criteria alone, and laboratory tests and x-rays may be unnecessary. But in some cases it needed.
- A normal erythrocyte sedimentation rate (ESR)
- The presence of bony outgrowths (osteophytes) on x-rays
- The presence of joint space narrowing on x-rays, indicating a loss of cartilage
Laboratory Tests
Laboratory tests may be recommended to help diagnose OA by ruling out conditions with similar symptoms.
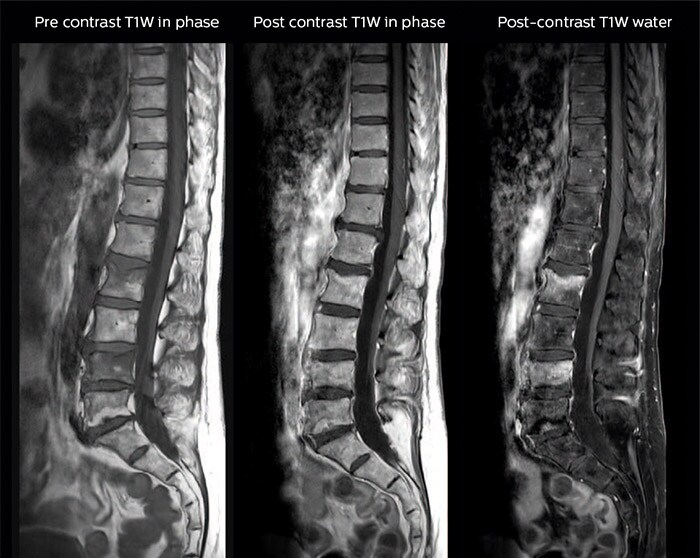
Imaging Tests
X-rays are often helpful for tracking the status of OA over time, but x-rays may appear normal during the early stages.
MRI imaging to confirm the condition associated with others condition.
References
[bg_collapse view=”button-orange” color=”#4a4949″ expand_text=”Show More” collapse_text=”Show Less” ]
- https://www.ncbi.nlm.nih.gov/pubmed/22632699
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3606549/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4233216/
- https://www.ncbi.nlm.nih.gov/pubmed/23147891
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4012322/
- https://www.ncbi.nlm.nih.gov/pubmed/23147891
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3290688/
- https://www.sciencedirect.com/topics/medicine-and-dentistry/osteoarthritis
- https://www.sciencedirect.com/topics/immunology-and-microbiology/osteoarthritis
- https://www.sciencedirect.com/journal/joint-bone-spine
- https://www.sciencedaily.com/releases/2018/10/181004110029.htm
- https://medlineplus.gov/osteoarthritis.html
- https://jamanetwork.com/journals/jama/fullarticle/186172
- https://www.practicalpainmanagement.com/spinal-osteoarthritis-spondylosis
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/osteoarthritis
- https://www.medicinenet.com/script/main/art.asp?articlekey=90187
- https://books.google.com/books/about/Osteoarthritis.html?id=YfFj8Gbq5H0C
- https://books.google.com/books/about/Osteoarthritis.html?id=4rI0CgAAQBAJ
- https://link.springer.com/chapter/10.1007/978-3-319-19560-5_4
- https://link.springer.com/article/10.1007/s11916-004-0075-z
- https://www.springer.com/kr/book/9783319195599
- https://www.webmd.com/osteoarthritis/qa/what-is-osteoarthritis-of-the-spine
- https://www.arthritis.org/about-arthritis/where-it-hurts/back-pain/causes/back-arthritis.php
- https://www.arthritis.org/about-arthritis/where-it-hurts/back-pain/causes/back-arthritis.php
[/bg_collapse]