Sleep paralysis is when during awakening or falling asleep, a person is aware but unable to move or speak. During an episode, one may hear, feel, or see things that are not there. It often results in fear. Episodes generally last less than a couple of minutes.It may occur as a single episode or be recurrent.
The condition may occur in those who are otherwise healthy, those with narcolepsy, or may run in families as a result of specific genetic changes. The condition can be triggered by sleep deprivation, psychological stress, or abnormal sleep cycles.The underlying mechanism is believed to involve a dysfunction in REM sleep. Diagnosis is based on a person’s description. Other conditions that can present similarly include narcolepsy, atonic seizure, and hypokalemic periodic paralysis.
A person experiencing sleep paralysis will find they are temporarily unable to move or speak when they wake up, or are falling asleep.
This paralysis can last from seconds to minutes. While it can be frightening, sleep paralysis is not harmful to the body or overall health
Or
A frightening form of paralysis that occurs when a person suddenly finds himself or herself unable to move for a few minutes, most often upon falling asleep or waking up. Sleep paralysis is due to an irregularity in passing between the stages of sleep and wakefulness.
Sleep paralysis is when, during awakening or falling asleep, a person is aware but unable to move or speak.During an episode, one may hear, feel, or see things that are not there. It often results in fear.Episodes generally last less than a couple of minutes. It may occur as a single episode or be recurrent.
Types of Sleep Paralysis
- Hypnagogic or predormital – when falling asleep
- Hypnopompic or post-dormital – when waking up
- Isolated sleep paralysis (ISP) – When ISP episodes are more frequent and cause clinically-significant distress and/or interference, it is classified as
- Recurrent isolated sleep paralysis(RISP) – Episodes of sleep paralysis, regardless of classification, are generally short (1–6 minutes), but longer episodes have been documented.With RISP the individual can also suffer back-to-back episodes of sleep paralysis in the same night, which is unlikely in individuals who suffer from ISP
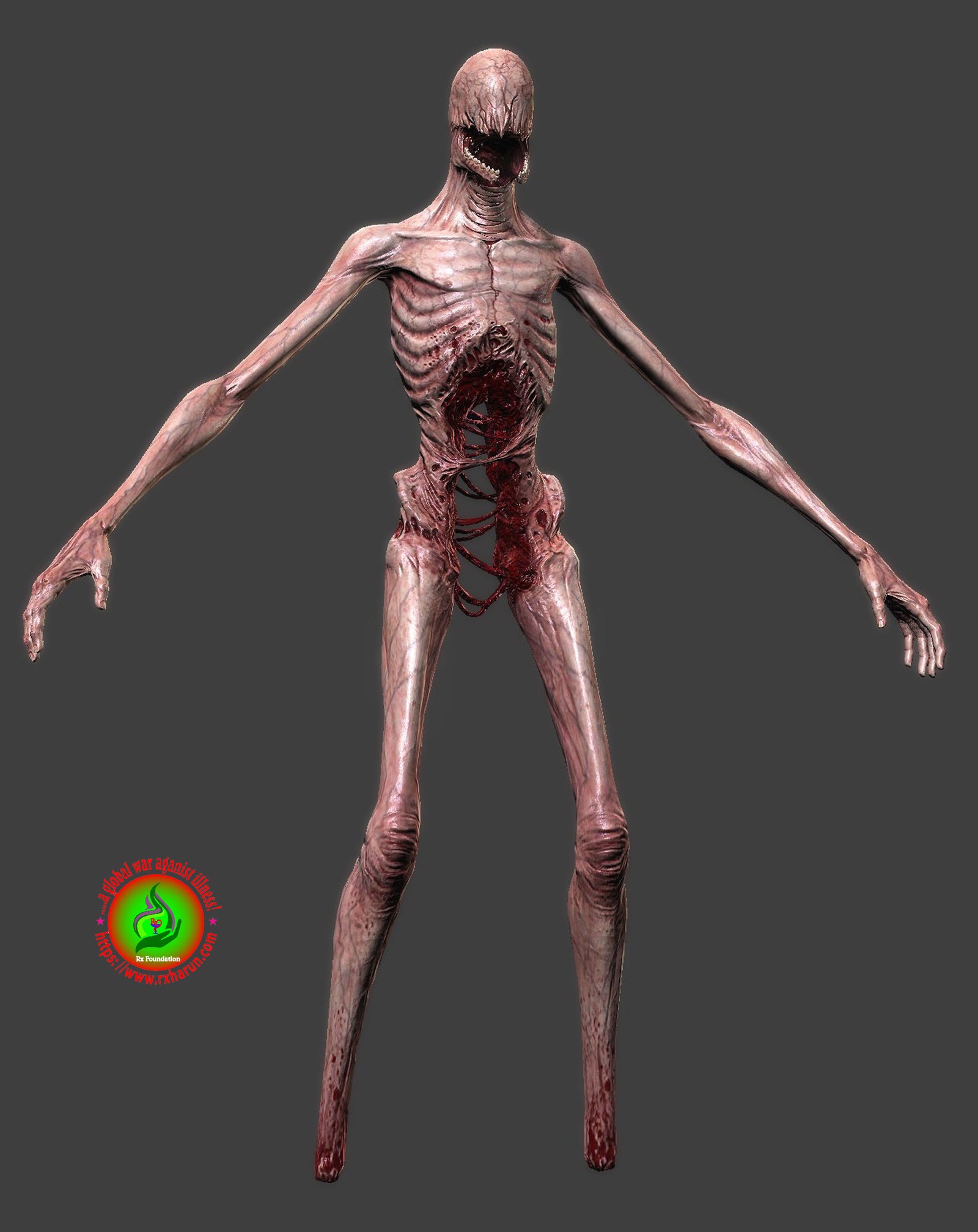
Types of Visions of Sleep Paralysis
The three main types of visions that have been linked to pathologic neurophysiology are
- Vestibular motor sensations,
- The incubus, and
- Believing there’s an intruder in the room.
Frequency
- Mild: Episodes occur less than once per month
- Moderate: Episodes occur more than once per month but less than weekly
- Severe: Episodes occur at least once per week
Duration
- Acute: 1 month or less
- Subacute: More than 1 month but less than 6 months
- Chronic: 6 months or longer
Risk Factors of Sleep Paralysis
The following can increase your chance of experiencing sleep paralysis
- Having a lack of sleep – If you’re sleep deprived, you may go straight into REM sleep, rather than slowly transitioning from light sleep to deep sleep, and not entering REM until the second half of the night.
- Having an irregular sleep pattern – Shift workers have been shown to be more likely to experience sleep paralysis.
- Age – Teenagers and young adults are most likely to experience sleep paralysis. It’s rare for someone to have their first experience after the age of 25.
- Certain sleeping positions – You’re much more likely to experience sleep paralysis when sleeping on your back. Some people who get regular sleep paralysis find that they only do so in a certain sleeping position, and that by avoiding this position they prevent sleep paralysis from occurring.
- Narcolepsy – Sleep paralysis represents one of the four classic symptoms of narcolepsy, a disorder that is associated with severe daytime sleepiness with an inability to stay awake. However not everyone who has narcolepsy will get it.
- Family history – Sleep paralysis is believed to run in families, but this has yet to be conclusively confirmed.
Who Gets Sleep Paralysis?
You aren’t the only one suffering from sleep paralysis. A study on 36,533 participants found that
- 7.6% of the general population
Students, psychiatric patients, Asian people, and women experience sleep paralysis more than their counterparts do.
- 28.3% of students
- 31.9% of psychiatric patients
Causes of Sleep Paralysis
As you begin to fall asleep, your body starts relaxing, taking you through the 4 stages of the non-rapid eye movement (NREM) phase, eventually lulling you into deep sleep. After 80 to 100 minutes, you move into the rapid eye movement (REM) phase, where you start dreaming vividly. You keep repeating this NREM/REM cycle till you wake up.
During the dream phase or the REM phase of your sleep, your brain paralyzes your muscles so that you don’t act out the dreams.During REM, your brain releases chemicals called glycine and GABA to paralyze your muscles5 so that you don’t physically act out the dreams. This state is called atonia. Your brain is highly active; your breathing is irregular; and your heart rate and blood pressure are high.
The basic cause of sleep paralysis is REM atonia
- REM stands for Rapid Eye Movement (the sleep phase linked with dreaming)
- Atonia means lack of muscle tension
- REM atonia is essential for healthy sleep, else you’d wreak havoc in your neighborhood by acting our your dreams on a nightly basis. This is no good for you, and no good for your neighbors.
- A lack of sleep
- A sleep routine that changes
- Mental health conditions such as stress or bipolar disorder
- Sleeping on the back
- Narcolepsy
- People who sleep on their back are more likely to experience sleep paralysis than sleeping in other positions.
- Use of certain medications such as those prescribed to treat ADHD
- Extreme physical fatigue.
- Overuse of stimulants
- A disruption of normal sleep patterns.
- A symptom of other sleep disorders such as narcolepsy.
- Irregular sleeping patterns, due, for example, to jet lag or shift work
- Sleeping on your back
- A family history of sleep paralysis
- Other sleep problems such as narcolepsy or night-time leg cramps
- Use of certain medications
- Substance abuse
- Mental conditions such as stress or bipolar disorder.
While Waking Up of Sleep Paralysis
Hypnopompic sleep paralysis occurs when you wake up before the REM stage is complete. This is due to an overlap in sleep states or an overlap between wakefulness and sleep. This can happen if
Nerves that make you sleep are hyperactive and those that wake you are underactive. So your brain delays in releasing your muscles.
- The group of nerve cells responsible for sleep – the REM sleep-on neurons – are hyperactivated.
- Or the group of nerve cells responsible for wakefulness and/or non-REM sleep – the REM sleep-off neurons – are underactive. This is because melatonin, the sleep hormone that regulates the sleep-off neurons, becomes lowest during REM sleep.8
- Or both these occur together.
Signs and Symptoms of Sleep Paralysis
Signs and symptoms include
- an inability to move the body when falling asleep or on waking, lasting for seconds or several minutes
- being consciously awake
- being unable to speak during the episode
- having hallucinations and sensations that cause fear
- feeling pressure on the chest
- having difficulty breathing
- feeling as if death is approaching
- sweating
- having headaches, muscle pains, and paranoia
- Be unable to move their arms and legs, body, and head when falling asleep or waking up
- Have episodes that last from only seconds to a few minutes
- It is also important to know if there is something else that is causing your sleep problems. They may be a result of one of the following
- Another sleep disorder such as narcolepsy
- A medical condition
- Medication use
- A mental health disorder
- Substance abuse
Treatment of Sleep Paralysis
Medical treatment starts with education about sleep stages and the inability to move muscles during REM sleep. People should be evaluated for narcolepsy if symptoms persist.The safest treatment for sleep paralysis is for people to adopt healthier sleeping habits.
However, in more serious cases tricyclic antidepressants or selective serotonin reuptake inhibitors (SSRIs) may be used.Despite the fact that these treatments are prescribed there is currently no drug that has been found to completely interrupt episodes of sleep paralysis a majority of the time
It’s also really important to avoid stress and anxiety, particularly before sleep. If you’re suffering from chronic stress, attend to that and your sleep paralysis could go away on its own.
- Relax your body into the paralysis – Don’t fight it forcefully, as this creates panic and increases the chance of having scary hallucinations.
- Try to gently wiggle your fingers and toes –These tiny movements will eventually tell your brain that your body is awake and to stop the atonia.
- Try to move your eyes – by blinking and looking around the room. Again, the goal is to establish waking-like movements to fully awaken your brain and body together.
- Try to move your lips and facial muscles.
- Focus on breathing as slowly and deeply as you can – If your breathing feels restricted, remember that you have been breathing fine like this while asleep for hours.
- Maintain a calm and positive mental state – Focus on relaxing thoughts. Imagine a beach in the sun, a million miles away from the darkness of your bedroom. Sing an upbeat song in your mind.
- Reappraisal of the meaning of the attack (cognitive reappraisal) – which entails closing one’s eyes, avoid panicking and re-appraising the meaning of the attack as benign.
- Psychological and emotional distancing (emotion regulation) – the sleeper reminds him- or herself that catastrophizing the event (i.e., fear and worry) will worsen and possibly prolong it;
- Inward focused-attention meditation – focusing attention inward on an emotionally salient positive object;
- Muscle relaxation – relaxing one’s muscles, avoid controlling breathing and avoid attempting to move.There are preliminary case reports supporting this treatment, although no randomized clinical trials yet to show its effectiveness.
- Cognitive-behavior therapy – Some of the earliest work in treating sleep paralysis was done using a culturally sensitive cognitive-behavior therapy called CA-CBT. The work focuses on psycho-education and modifying catastrophic cognitions about the sleep paralysis attack. This approach has previously been used to treat sleep paralysis in Egypt, although clinical trials are lacking
- Emotional and Psychological Distancing – Sleepers remind themselves that, because the attack is common, benign and temporary, they shouldn’t be scared or worried. Fear and worry only make the attack scarier and possibly longer.
- Meditating: – Sleepers focus attention inward, on a strong and emotionally positive “internal object” (i.e. a thought), such as a memory of a loved one or a happy moment, or comforting prayer. They concentrate fully on and actively engage with the thought, and ignore any external stimuli, i.e., hallucinations.
- Getting six to eight hours of sleep a night (if you currently sleep less)
- Medications to treat bipolar disorder or another mental health disorder
- Treatment for underlying conditions, such as leg cramps
Maintain these goals for the duration of the sleep paralysis and stay on top of any fear.
Tips for better sleep
There is no specific treatment for sleep paralysis, but stress management, maintaining a regular sleep schedule, and observing good sleep habits can reduce the likelihood of sleep paralysis.
Strategies for improving sleep hygiene include:
- keeping bedtime and wake-up time consistent, even on holidays and weekends
- ensuring a comfortable sleep environment, with suitable bedding and sleepwear and a clean, dark and cool bedroom
- reducing light exposure in the evening and using night-lights for bathroom trips at night
- getting good daylight exposure during waking hours
- not working or studying in the bedroom
- avoiding napping after 3.00 p.m. and for longer than 90 minutes
- not eating a heavy evening meal, or eating within 2 hours of going to bed
- not sleeping with the lights or television on
- abstaining from evening alcohol or caffeine products
- exercising daily, but not within 2 hours of bedtime
- including a calming activity in the bedtime ritual, such as reading or listening to relaxing music
- leaving phones and other devices outside the bedroom
- putting electronics aside at least 1 hour before going to bed
- managing any depression or anxiety disorder
- reducing intake of stimulants
- practicing meditation or regular prayer
- not sleeping on your back
Understanding the physiology of sleep and the mechanism for sleep paralysis is an important step to overcoming it.
Home Treatment of Sleep Paralysis
If you are having trouble sleeping, check out this article on changing up your bedtime routine to promote better sleep.
- If at all possible, try to go to bed around the same time every night.
- Wake up around the same time every morning.
- Sleep on your side instead of on your back.
- Keep your dinner light. Save heavy proteins and fats for earlier in the day (if, of course, they’re healthy fats!).
- Avoid sugar in the evening, as this can be troublesome for the body.
- Avoid caffeine and alcohol in the evening. Caffeine, as we all know, can make it more difficult to fall asleep. Alcohol can disrupt normal sleep cycles, even though it makes you feel drowsy.
- Meditate before you go to bed. Even five minutes can have a positive effect. But if you’re really struggling to wind down, go for 20 minutes or even half an hour. Meditation takes practice to really get you in that zen place, but it’s worth it, and can ease any nighttime (and daytime) anxiety significantly.
- Avoid electronics for at least half an hour before you go to sleep. The blue light can lead to sleep disruptions. Also, turn off any electronics that you may have running in your bedroom.
- Try drinking some chamomile tea before bed.
- Ask your doctor about whether valerian root or melatonin supplements may be safe and effective for your individual health.
- If you’re experiencing a great deal of stress or other mental issues on a chronic basis, consider seeing a therapist or counselor to help you arrive at effective solutions to underlying problems.
References
[bg_collapse view=”button-orange” color=”#4a4949″ expand_text=”Show More” collapse_text=”Show Less” ]
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2921144/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2637172/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5167075/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3156892/
[/bg_collapse]



Visitor Rating: 5 Stars