Spina bifida is a birth defect where there is incomplete closing of the backbone and membranes around the spinal cord. The most common location is the lower back, but in rare cases, it may be the middle back or neck. Occulta has no or only mild signs. Signs of occult may include a hairy patch, dimple, dark spot, or swelling on the back at the site of the gap in the spine. Meningocele typically causes mild problems with a sac of fluid present at the gap in the spine. Myelomeningocele, also known as open spina bifida, is the most severe form.
Types of Spina Bifida
There are four main types of spina bifida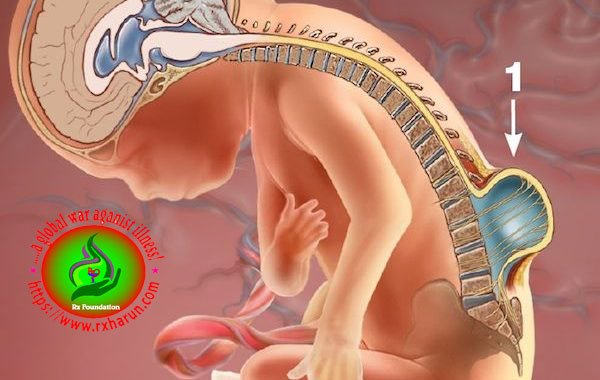
- Occulta – This is the mildest form. Most patients have no neurological signs or symptoms. There may be a small birthmark, dimple or tuft of hair on the skin where the spinal defect is. The person may never know they have spina bifida unless a test for another condition reveals it by chance.
- Closed neural tube defects – In this version, there can be a variety of potential defects in the spinal cord’s fat, bone, or meninges. In many cases, there are no symptoms; however, in some, there is partial paralysis and bowel and urinary incontinence.
- Meningocele – The spinal cord develops normally, but the meninges, or protective membranes around the spinal cord, push through the opening in the vertebrae. The membranes are surgically removed, usually with little or no damage to nerve pathways.
- Myelomeningocele – Myelomeningocele is the most severe form of spina bifida. In this condition, the spinal cord is exposed, causing partial or complete paralysis of the body below the opening. The symptoms are outlined in detail below.
Causes of Spina Bifida
We’re not sure exactly what causes spina bifida, but these things may play a role
Ethnic group – This is a group of people, often from the same country or region, who share language or culture. Spina bifida and other NTDs are more common in Caucasians and Hispanics and less common among Ashkenazi Jews, most Asian groups and African- Americans.
Folic acid – Folic acid is a B vitamin that every cell in your body needs for normal growth and development. Taking 400 micrograms of folic acid every day before and during early pregnancy can help reduce your baby’s risk for NTDs. You need folic acid when you’re pregnant, too. During pregnancy, take a prenatal vitamin each day that has 600 micrograms of folic acid in it.
Genes – Genes are the part of your body’s cells that store instructions for the way your body grows and works. Genes are passed from parents to children. Sometimes changes in genes can cause conditions like spina bifida. Parents can pass these gene changes to their children. You may be more likely than others to have a baby with spina bifida if
- You or your partner has spina bifida. When one parent has spina bifida, there’s a 1 in 25 (4 percent) chance of passing spina bifida to your baby.
- You already have a child with spina bifida. In this case, there’s a 1 in 25 (4 percent) chance of having another baby with spina bifida.
Health conditions
Health conditions and medicines you take during pregnancy may play a role in causing spina bifida
- Get to a healthy weight before pregnancy.
- Get treatment for health conditions, like diabetes.
- Tell your provider about any medicines and supplements you take. This includes any prescription and over-the-counter medicines, supplements and herbal products. Your provider may tell you to stop taking a medicine or switch you to one that’s safer during pregnancy. For example, some anti-seizure medicines may increase your risk of having a baby with an NTD
Getting overheated during pregnancy
This may increase your chances of having a baby with spina bifida. Don’t use hot tubs or saunas when you’re pregnant. If you have a fever, take acetaminophen (Tylenol®) right away and call your provider.
What health problems can spina bifida causes
Spina bifida can cause a number of health problems, including
Chiari II malformation
This condition happens when the lower part of the brain sits in the upper part of the neck. Some babies with this condition have hydrocephalus (fluid buildup in the brain), weakness in the upper body (like in the arms and hands) and/or breathing or swallowing problems. Babies with this condition usually have myelomeningocele.
Hydrocephalus
Extra fluid can cause the head to swell and put pressure on the brain. Hydrocephalus can cause intellectual and developmental disabilities. These are problems with how the brain works that can cause a person to have trouble or delays in physical development, learning, communicating, taking care of himself or getting along with others. In some cases, a surgeon needs to drain the extra fluid from a baby’s brain.
Latex allergy
Many babies with spina bifida are allergic to latex (natural rubber). If your baby is allergic to latex, keep him away from items made of latex like rubber nipples and pacifiers.
Learning disabilities
Children with spina bifida sometimes have problems with language, reading, math and paying attention.
Meningitis
This is an infection of the meninges that causes swelling in the brain and spinal cord. Meningitis can damage the brain and can be life-threatening. If your baby has meningitis, she may need antibiotics (medicine that kills infections caused by bacteria).
Paralysis
People with spina bifida higher on the spine may have paralyzed legs or feet and need to use wheelchairs. Those with spina bifida lower on the spine (near the hips) may have more use of their legs. They may be able to walk on their own or use crutches, braces or walkers to help them walk. Some babies can start exercises for the legs and feet at an early age to help them walk with braces or crutches when they get older.
Skin problems
People with spina bifida can develop sores, calluses, blisters, and burns on their feet, ankles and hips. But they may not know they have these problems because they may not be able to feel certain parts of their body. Your baby’s provider can recommend ways to help prevent skin problems.
Tethered spinal cord
This condition happens when the spinal cord is held tightly in place, causing the cord to stretch as your baby grows. The stretching can cause nerve damage in the spine. Babies with a tethered spinal cord may have problems like back pain and a curved spine (also called scoliosis). The tethered spinal cord can be treated with surgery. This condition affects babies with myelomeningocele, meningocele and spina bifida occult.
Urinary tract infections (also called UTIs)
The urinary tract is the system of organs (including the kidneys and bladder) that helps your body get rid of waste and extra fluids in the urine. Babies with spina bifida often can’t control when they go to the bathroom because the nerves that help a baby’s bladder and bowels work are damaged. If your baby has problems emptying the bladder completely, this can cause UTIs and kidney problems. Your baby’s health care provider can teach you how to use a plastic tube called a catheter to empty your baby’s bladder.
Symptoms of Spina Bifida
- Cognitive symptoms – Awareness, thinking, learning, judging and knowing are known as cognition. Problems in the neural tube can have a negative impact on brain development. If the brain’s cortex, and especially the frontal part, does not develop properly, cognitive problems can arise.
- Type 2 Arnold-Chiari malformation – This is an abnormal brain development involving a part of the brain known as the cerebellum. This may cause hydrocephalus. It can affect language processing and physical coordination.
- Learning difficulties – People with spina bifida have normal intelligence. However, learning difficulties can occur, leading to problems with attention, solving problems, reading, understanding spoken language, making plans, and grasping abstract concepts.
- Coordination – There may also be problems with visual and physical coordination. Doing up buttons or shoelaces can be difficult.
- Paralysis – Most patients have some degree of paralysis in their legs. In cases of partial paralysis, leg braces or a walking stick may be necessary. A person with total paralysis will need a wheelchair. If the lower limbs are not exercised, they can become weak, leading to dislocated joints and misshapen bones.
- Bowel and urinary incontinence – These are common.
- Meningitis – There is a higher risk of meningitis among people with spina bifida. This can be life-threatening.
- Other problems – In time, the individual may experience skin problems, gastrointestinal problems, latex allergies, and depression.
Diagnosis of Spina Bifida
- Maternal serum alpha-fetoprotein (MSAFP) test – For the MSAFP test, a sample of the mother’s blood is drawn and tested for alpha-fetoprotein (AFP) — a protein produced by the baby. It’s normal for a small amount of AFP to cross the placenta and enter the mother’s bloodstream. But abnormally high levels of AFP suggest that the baby has a neural tube defect, such as spina bifida, though some spina bifida cases don’t produce high levels of AFP.
- Test to confirm high AFP levels – Varying levels of AFP can be caused by other factors — including a miscalculation in fetal age or multiple babies — so your doctor may order a follow-up blood test for confirmation. If the results are still high, you’ll need further evaluation, including an ultrasound exam.
- Other blood tests – Your doctor may perform the MSAFP test with two or three other blood tests. These tests are commonly done with the MSAFP test, but their objective is to screen for other abnormalities, such as trisomy 21 (Down syndrome), not neural tube defects.
- A prenatal test measures the level of maternal serum alpha-fetoprotein (MSAFP, or AFP), which is unusually high in women carrying a fetus with spina bifida or another neural tube defect.
- This test usually is done as one of 3 tests known together as the “triple screen.” The triple screen includes AFP, ultrasound, and testing of amniotic fluid.
- Any pregnant woman who has a high level of AFP should undergo 2 additional tests that are very accurate in detecting severe spina bifida: ultrasound of the fetal spine and testing of the amniotic fluid for AFP.
- Amniotic fluid is the fluid that surrounds the fetus in the womb. A small amount of the fluid is removed through a large needle and tested in various ways that might indicate abnormalities in the fetus. Removal of amniotic fluid is a safe, routine procedure called amniocentesis.
Treatment of Spina Bifida
Treatment depends on several factors, mainly how severe the signs and symptoms are.
Surgical options
- Surgery to repair the spine – This can be done within 2 days of birth. The surgeon replaces the spinal cord and any exposed tissues or nerves back into the newborn’s body. The gap in the vertebrae is then closed and the spinal cord sealed with muscle and skin. If bone development problems occur later, such as scoliosis or dislocated joints, further corrective surgery may be needed. A back brace can help correct scoliosis.
- Prenatal surgery – The surgeon opens the uterus and repairs the spinal cord of the fetus, usually during week 19 to 25 of pregnancy. This type of surgery may be recommended to reduce the risk of spina bifida worsening after delivery.
- Cesarian-section birth – If spina bifida is present in the fetus, delivery will probably be by cesarean section. This is safer for the exposed nerves.
- Hydrocephalus – Surgery can treat a buildup of cerebrospinal fluid in the brain. The surgeon implants a thin tube, or shunt, in the baby’s brain. The shunt drains away excess fluid, usually to the abdomen. A permanent shunt is usually necessary.
Physical and occupational therapy
- Physical therapy – This is vital, as it helps the individual become more independent and prevents the lower limb muscles from weakening. Special leg braces may help keep the muscles strong.
- Assistive technologies – A patient with total paralysis of the legs will need a wheelchair. Electric wheelchairs are convenient, but manual ones help maintain upper-body strength and general fitness. Leg braces can help those with partial paralysis. Computers and specialized software may help those with learning problems.
- Occupational therapy – This can help the child perform everyday activities more effectively, such as getting dressed. It can encourage self-esteem and independence. Treatment for urinary incontinence – A urologist will carry out an assessment and recommend appropriate treatment.
- Clean intermittent catheterization (CIC) – This is a technique to empty the bladder at regular intervals. The child or a parent or carer learns to place the catheter through the urethra and into the bladder to empty it.
- Anticholinergics – These drugs are normally prescribed for adults with urinary incontinence, but a doctor child may prescribe it for a child. They increase the amount of urine the bladder can hold and reduce the number of times the child has to pee.
- Botox injection – If the child’s bladder contracts abnormally, known as a hyper-reflexes bladder, the doctor may recommend a botulinum toxin (Botox) injection to paralyze the muscles. If it works, treatment will be repeated every 6 months.
- Artificial urinary sphincter (AUS) – This surgically implanted device has a silicone cuff, surrounded by a liquid, a pump, and a balloon. It is attached to the urethra and the balloon is placed in the abdomen. The pump is placed under the skin of the scrotum in males and under the skin of the labia in females. When the child wants to urinate they press the pump, which temporarily empties the fluid from the cuff into the balloon, releasing the pressure on the cuff and opening the urethra, allowing urine to be released. It may not be suitable for younger boys who have not yet reached puberty.
- Mitrofanoff procedure – The surgeon removes the appendix and creates a small channel, the Mitrofanoff channel, which ends at an opening, or stoma, just below the belly button. The child can place a catheter into the stoma to release urine and empty the bladder.
References
[bg_collapse view=”button-orange” color=”#4a4949″ expand_text=”Show More” collapse_text=”Show Less” ]
- https://www.ncbi.nlm.nih.gov/pubmed/15555669
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4898641/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5327787/
- https://www.ncbi.nlm.nih.gov/pubmed/28734746
[/bg_collapse]
