Infraspinatus Tendinopathy is a tendon that attaches muscle to bone and is the focus of the “pull” of the muscle. When you damage it the muscle pulls part of the tendon away from the bone and the attachment point (or focus) becomes frayed and sore. While the tendons themselves are enormously strong (half the tensile strength of steel), the attachment to the bone is usually weaker and first to give. Tendinitis is very common at the shoulder. Only selected arm/shoulder movements hurt, the worst being putting your hand in your back pocket.
The Infraspinatus muscle is one of the four rotator cuff muscles of the shoulder, with the primary function of stabilization of the glenohumeral (GH)l joint. Infraspinatus pain often presents as pain on the front side of the shoulder. Infraspinatus muscle and tendon pain began oftentimes without trauma, dubbed as an “overuse” injury. The infraspinatus is the second most commonly torn muscle/tendon in the shoulder.
Anatomy of Infraspinatus Tendinopathy
The Infraspinatus muscle is one of the four muscles that make up the rotator cuff, the others being: supraspinatus, teres minor and subscapularis.
- Origin – infraspinatus fossa of the scapula
- Insertion – middle facet of the greater tubercle of the humerus
- Innervation – suprascapular nerve (C5-6)
- Arterial supply – suprascapular and circumflex scapular arteries1
- Action – external rotation of the humerus
- Origin – It arises medially from the infraspinous fossa of the scapula, specifically from fleshy fibers from its medial two-thirds, and by tendinous fibers from the ridges on its surface; it also arises from the infraspinatus fascia which covers it and separates it from the teres major and minor muscles.
- Insertion – The fibers converge to a tendon, which glides over the lateral border of the spine of the scapula, and, passing across the posterior part of the capsule of the shoulder joint, is inserted into the middle facet of the greater tubercle of the humerus.
- Relations – The tendon of this muscle is sometimes separated from the capsule of the shoulder joint by a bursa, which may communicate with the joint cavity.
- Innervation – The infraspinatus muscle is supplied by the suprascapular nerve (C5 and C6), which arises from the superior trunk of the brachial plexus and passes laterally through the posterior triangle of the neck and through the scapular notch on the superior border of the scapula. After supplying fibers to the supraspinatus muscle, it supplies articular branches to the capsule of the shoulder joint.
- Action – It acts with teres minor to externally rotate the glenohumeral joint, and with other rotator cuff muscles to stabilize the shoulder.
Causes of Infraspinatus Tendinopathy
- Sudden forceful fall down
- Road traffic accident
- Falls – Falling onto an outstretched hand is one of the most common causes of tendinitis.
- Sports injuries – Many Injury occurs during contact sports or sports in which you might fall onto an outstretched hand — such as in-line skating or snowboarding.
- Motor vehicle crashes – Motor vehicle crashes can cause necks of femur fracture to break, sometimes into many pieces, and often require surgical repair.
- Have osteoporosis – a disease that weakens your bones
- Eave low muscle mass or poor muscle strength – or lack agility and have poor balance (these conditions make you more likely to fall)
- Walk or do other activities in the snow or on the ice – or do activities that require a lot of forwarding momenta, such as in-line skating and skiing
- Wave an inadequate intake of calcium or vitamin D
- Football or soccer, especially on artificial turf
- Rugby
- Horseback riding
- Hockey
- Skiing
- Snowboarding
- In-line skating
Symptoms of Infraspinatus Tendinopathy
Acute Stage
There are a few different symptoms that are possible
- Pain radiating into the neck and upper back areas and down into biceps
- Inability to raise the arm above head because of stiffness and feeling numb
- Weakness in the shoulder
- Discomfort with sleep when rolling onto side
- However, the most common presentation is shoulder pain or discomfort. This may occur with activity, particularly shoulder activity above the horizontal position, but may also be present at rest in bed.
- Pain-restricted movement above the horizontal position may be present, as well as weakness with shoulder flexion and abduction.
- Severe pain that might worsen when gripping or squeezing or moving.
- Inability to move immediately after a fall
- Inability to put weight on your hand on the side of your injured thighs.
- Stiffness, bruising and swelling in and around your shoulder area
- Shorter leg on the side of your injured shoulder.
- Turning outward of your hand on the side of your injured
- Swelling
- Tenderness
- Bruising
Chronic Stage
- You have Pain in the shoulder when doing a repetitive shoulder activity that eventually becomes noticeable when the shoulder is at rest.
- You are experiencing Atrophy (loss of Range of Motion)or weakening of the tendons and muscles in the rotator cuff.
- You have pain that starts as a dull ache and progresses to radiating pain from the shoulder, especially when sleeping.
- You have Sudden pain when reaching above the head or bringing the arm out to the side.
- You are experiencing Muscle spasm and weakness in the arm and shoulder area with a limited range of motion.
- You are experiencing a crackling sensation that may be felt as the condition worsens.
Direct signs are
- Non-visualization of the supraspinatus tendon
- Hypoechoic discontinuity in tendon
Indirect signs are
- Double cortex sign
- Sagging peribursal fat sign
- Compressibility
- Muscle atrophy
Secondary associated signs are
- Cortical irregularity of greater tuberosity
- Shoulder joint effusion
- Fluid along the biceps tendon
- Fluid in the axillary pouch and posterior recess
Diagnosis of Infraspinatus Tendinopathy
- Full-thickness rotator cuff tear (FTRCT)
- Complete cuff tear: full-thickness as well as full-width tear
- Vertical with a connection from joint to the bursa, not involving the whole breadth of the tendon
- Partial-thickness rotator cuff tear (PTRCT) bursal surface tear and articular surface tear
- Critical zone tear partial or full-thickness
- Rim rent tear: articular surface tear of the footprint
- Intratendinous tear / central tears: not in communication with the joint surface or with the bursal surface of the tendon; also known as tendon delamination or interstitial tear; if the gap is filled with fluid then it is called cleavage tear of the rotator cuff tendon
Radiographic Features
Exact features depend on the type of tear, general features include Typically these are normal in acute tears with chronic tears showing degenerative-type changes
- May show a decreased acromiohumeral interval
- < 7 mm on true AP shoulder radiograph in chronic tears
- < 2 mm on an ‘active abduction’ view in acute tears
- May show decreased infraspinatus opacity and decreased bulk due to fatty atrophy in chronic tears
- Humeral subluxation superiorly may be seen in chronic tears
- May show features of acromial impingement
- spur formation on the undersurface of acromioclavicular joint
- acromion with an inferolateral tilt seen on outlet view (i.e. modified ‘Y’ view)
- type III acromion
- Secondary degenerative changes: sclerosis, subchondral cysts, osteolysis, and notching/pitting of greater tuberosity
Ultrasound
- In the hands of a good radiologist, ultrasound may have up to 90% sensitivity and specificity. It can also reveal other mimics like tendinosis, calcific tendinitis, subacromial-subdeltoid bursitis, greater tuberosity fracture, and adhesive capsulitis.
- Full-thickness tears extend from bursal to the articular surface, while partial-thickness tears are focal defects in the tendon that involve either the bursal or articular surface. Full-thickness appear on ultrasound as hypoechoic/anechoic defects in the tendon. Due to the fluid replacing tendon, cartilage shadow gets accentuated giving a ‘double cortex’ or ‘cartilage interface sign.
MRI
- Complete tears are easier to diagnose on MRI than a full-thickness tear. Hyperintense signal area within the tendon on T2W, fat-suppressed and GRE sequences, usually corresponding to fluid signal is seen.
- Clinical judgment, rather than over-reliance on MRI or any other modality, is strongly advised in determining the cause of shoulder pain, or planning its treatment since rotator cuff tears are also found in some without pain or symptoms.
- The role of X-ray, MRI, and ultrasound, is adjunctive to clinical assessment and serves to confirm a diagnosis provisionally made by a thorough history and physical examination. Over-reliance on imaging may lead to overtreatment or distract from the true dysfunction causing symptoms.[rx]
Test 1: Resisted Lateral Rotation
 Have the client stand with her legs at least shoulder-width apart so she is stable while doing the test. Place one hand on her upper arm just above the elbow and press the upper arm into the body for stability. With the person’s arm bent in front at a right angle, place your other hand on the outside of her lower arm just above the wrist. Now ask the client to push laterally or outward toward you while you resist the push with equal force (Image 1A). This test is done at 90 degrees to the body, first, but also may need to be done at 30 degrees (Image 1B) and at 135 degrees (Image 1C) for more precise testing. The different angles put stress on different parts of the tendon. A positive test, when pain is felt, indicates that the infraspinatus is injured.
Have the client stand with her legs at least shoulder-width apart so she is stable while doing the test. Place one hand on her upper arm just above the elbow and press the upper arm into the body for stability. With the person’s arm bent in front at a right angle, place your other hand on the outside of her lower arm just above the wrist. Now ask the client to push laterally or outward toward you while you resist the push with equal force (Image 1A). This test is done at 90 degrees to the body, first, but also may need to be done at 30 degrees (Image 1B) and at 135 degrees (Image 1C) for more precise testing. The different angles put stress on different parts of the tendon. A positive test, when pain is felt, indicates that the infraspinatus is injured.

Image 1B: Rotate client’s arm inward to 30 degrees and repeat test for more precise results

Image 1C: Rotate client’s arm outward to 135 degrees and repeat test for more precise results
Test 2: Passive Elevation
First, say to the client, “Raise your arm above your head.” This test is to see if the person can actually raise her arm. Then place one hand on the elbow and your other hand at the back of the same shoulder to stabilize the joint. Now push the arm back behind the client’s head diagonally until you come to the very end of the range of movement (Image 2). If there is still no pain, give the arm a slight jerk in the same direction. This jerk is always done at the very end of the range of motion, and the person is totally relaxed while you passively test the arm. Pain on this test indicates that the deep distal end is injured.

Image 2: Passive elevation test
Test 3: The Painful Arc Test
Ask the client to lift the arm slowly out to the side until the arm is raised above the head. Instruct the client to stop if there is any pain and then to continue the motion to see if the pain ceases. Pain on this test between 70 degrees and 110 degrees indicates that the superficial distal end of the infraspinatus tendon is injured.
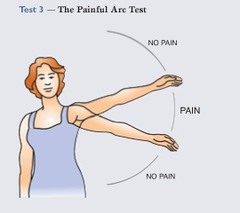
Image 3: Painful arc test
Two to three months of rest will sometimes allow infraspinatus tendinitis to heal, but more often it will remain for years, especially in an active person. The tendon injury exercise program, along with rest, may improve the condition. Treatment is usually recommended if rest and exercise don’t eliminate the pain in the course of a month. Hitting backhand in racquet sports is not a good idea while the client is in treatment, nor are any exercises that cause pain. Push-ups and chin-ups are two of the worst offenders when this injury is present. Here is a description of four treatment options.
Treatment of Infraspinatus Tendinopathy
Many different options are reported in the literature for treating calcific tendinopathy of the rotator cuff. Treatment of this condition can be conservative or surgical.
- Iontophoresis with acetic acid – The first application of this technique in orthopedics was described by Beutel and Clementshitsch [rx]. Iontophoresis involves the use of an electrode inserted in a sponge which increases the absorption, through the skin, of a drug, in this case, acetic acid. The use of acetic acid is based on the concept that the hydroxyapatite crystals are soluble in solutions with an acid pH. Leduc et al. [rx] compared the results obtained in patients treated with physical therapy (PT) and iontophoresis with acetic acid with those obtained in patients treated with PT and iontophoresis with placebo. The study failed to provide clear significant results in support of the use of acetic acid iontophoresis.
- Extracorporeal shock wave therapy – Extracorporeal shockwave therapy (EWST), which involves applying pressure waves to the surface of the skin. This may promote the regeneration of tissue and speed up the healing process. EWST has been shown to be effective for some lower limb conditions. Several studies have demonstrated the efficacy of extracorporeal shock wave therapy (SWT), either radial (SWT) or focal (SWT), in rotator cuff calcific tendinopathy [rx, rx]. ESWT is based on the use of single pressure pulses, or shock waves. By means of US or radiographic guidance, these are focused on the calcification. The use of rESWT has been reported to give satisfactory results, but to date, there are no level-1 reports in the literature. Lee et al. [rx], in a systematic review, reported moderate evidence supporting the use of SWD.
- Massage – Massage alone is not usually an effective treatment for infraspinatus tendinitis. There is often very stubborn scar tissue that needs to be broken down as described below. Massage of the infraspinatus muscle is useful as an adjunct to friction and exercise therapy.
- Friction Therapy – If the tendon tear is not too widespread, then four to six weeks of friction treatment are usually effective. Friction therapy reduces adhesive tissue and helps the tendon to heal correctly. The therapy should not be painful, just a little annoying.
- Weighted pendulum exercise – Sit or stand holding a 5- to 10-pound weight in the hand of the affected shoulder. Use a hand weight or make one from a gallon container filled with water. Relax the shoulder, and allow the arm to hang straight down. Lean forward at a 20- to a 25-degree angle (if you’re standing, bend your knees slightly for a base of support), and swing your arm gently in a small circle, about one foot in diameter. Perform 10 circles in each direction, once or twice a day. As symptoms improve, you can make the circle wider — but never force it.
- Towel stretch – Grasp a dishtowel behind your back and hold it at a 45-degree angle. Use your good arm to gently pull the affected arm up toward the lower back. Do this stretch 10 to 20 times per day. You can also perform this exercise while holding the towel horizontally.
- Cross-body stretch – Sitting or standing, use the unaffected arm to lift the affected arm at the elbow and bring it up and across your body. Press gently, just above the elbow, to stretch the shoulder. Hold the stretch for 15 to 20 seconds. Do this exercise 10 to 20 times per day.
- Finger walk – Stand facing a wall at a distance of about three-quarters of an arm’s length away. With the affected arm, reach out and touch the wall at about waist level. Slowly walk your fingers up the wall, spider-like, as far as you comfortably can or until you raise your arm to shoulder level. Your fingers should be doing most of the work, not your shoulder muscles. Keep the elbow slightly bent. Slowly lower the arm — with the help of your good arm, if necessary. Perform this exercise 10 to 20 times a day. You can also try this exercise with the affected side facing the wall.
- Isometric muscle toning exercises – Heat and stretch your shoulder joint before doing these exercises. Use flexible rubber tubing, a bungee cord, or a large rubber band to provide resistance.
- Inward rotation – Hook or tie one end of the cord or band to the doorknob of a closed door. Holding your elbow close to your side and bent at a 90-degree angle, grasp the band (it should be neither slack nor taut) and pull it in toward your waist, like a swinging door. Hold for five seconds.
- Outward rotation – Hold your elbows close to your sides at a 90-degree angle. Grasp the band in both hands and move your forearms apart two to three inches. Hold for five seconds. Do 15 to 20 sets of these exercises each day.
Medication
- Antibiotic – Cefuroxime or Azithromycin, or Flucloxacillin or any other cephalosporin/quinolone antibiotic must be used to prevent infection or clotted blood remove to prevent furthers swelling and edema. Antibiotics and tetanus vaccination may be used if the bone breaks through the skin creating immunization.
- NSAIDs – Prescription-strength drugs that reduce both pain and inflammation. Pain medicines and anti-inflammatory drugs help to relieve pain and stiffness, allowing for increased mobility and exercise. There are many common over-the-counter medicines called non-steroidal anti-inflammatory drugs (NSAIDs). They include and Ketorolac, Aceclofenac, Naproxen, Etoricoxib.
- Corticosteroids – Also known as oral steroids, these medications reduce inflammation. Corticosteroid injections around the tendon can reduce short-term pain and swelling. However, they may also make relapse more likely and can sometimes impair collagen production.
- Muscle Relaxants – These medications provide relief from associated muscle spasms or injury
- Neuropathic Agents – Drugs(pregabalin & gabapentin) that address neuropathic—or nerve-related—pain. This includes burning, numbness, and tingling.
- Opioids – Also known as narcotics, these medications are intense pain relievers that should only be used under a doctor’s careful supervision.
- Topical Medications – These prescription-strength creams, gels, ointments, patches, and sprays help relieve pain and inflammation through the skin.
- Calcium & vitamin D3 – To improve bone health and healing fracture. As a general rule, men and women age 50 and older should consume 1,200 milligrams of calcium a day, and 600 international units of vitamin D a day.
- Glucosamine & Diacerein, Chondroitin sulfate – can be used to tightening the loose tendon, cartilage, ligament, and cartilage, ligament regenerates cartilage or inhabits the further degeneration of cartilage, ligament.
- Dietary supplement -to remove general weakness & healing and improved health.
- Antidepressants – A drug that blocks pain messages from your brain and boosts the effects of endorphins (your body’s natural painkillers).
- Menthol – provides deep penetrating pain relief with a nice cooling sensation
- Vitamin B1, B6, B12– promotes normal nerve function
- Vitamin E – anti-inflammatory, enhances circulation, hydrates the skin
- Aloe vera – anti-inflammatory properties, soothes the skin
- Tea Tree – enhances the penetration of ingredients
- MSM – supports healthy connective tissues, anti-inflammatory
- Ilex Leaf Extract – increases circulation, skin conditioner
- Platelet-rich plasma (PRP) injections – involve injecting plasma from the person’s blood into areas around the tendon. Platelets promote cell repair and healing. PRP injections are more effective in this case and use in three treatments administered at two-week intervals. All previous treatments in this patient had failed. Symptoms regressed within six weeks and the benefit was maintained at one year.
- Steroid injections and percutaneous needling– Subacromial steroid injection and percutaneous needling are treatments often applied in rotator cuff calcific tendinopathy [rx–rx]. They are inexpensive and relatively easy to perform and carry a low risk of complications. Percutaneous needling is more invasive involving the use of a needle for the infiltration of lidocaine and the aspiration of the calcific material. The procedure is performed under the supervision of health.
Surgical Treatment
- Two types of surgical treatment are available: open surgery and arthroscopic treatment [rx]. The arthroscopic technique consists of an articular stage and a subacromial stage. After a glenohumeral inspection, the subacromial stage is performed through the posterior and lateral portals. After bursal debridement, the calcium deposits are localized by percutaneous needling. Residual calcification is than excised using a resector and curettes.
- Approximately 10% of patients are resistant to conservative treatment and therefore need surgery to remove the calcium deposits [rx]. Surgery is indicated in patients with severe symptoms persisting for more than six months [rx].
Location and Friction of the Infraspinatus Tendon
The client is lying on her side on the table with the injured side up. The injured arm hangs off the table at shoulder level. Run your finger outward along the spine of the scapula (the bony ridge that separates the upper and lower scapula). As you reach the lateral end of the spine of the scapula, drop down about a half inch to the medial aspect of the greater tubercle of the humerus; this is the most common site of injury. Move horizontally across the arm to apply transverse friction with the thumb or forefinger for 10–12 minutes (Image 4). Take a break after five or six minutes to give both of you a rest.

Image 4: Applying transverse friction to the infraspinatus tendon
Exercise Therapy
This tendon exercise program is very effective if done daily for six to eight weeks.1 The stretching realigns the scar tissue fibers so they can heal correctly, and the weight-calibrated exercises systematically increase the strength of the tendon. If the client’s personality is such that she will not do it consistently, this is not the program to recommend. In these cases, try only giving the client strengthening exercises. There are five steps to the program: warm-up, stretch, exercise, stretch, and ice or heat.
- First, have the client warm up the tendon by circling the arm for two or three minutes. Ask her to stand with the arm 3 or 4 inches in front of the body and make a wide, slow circle.
- Stretch the tendon five times for 30 seconds each time. This stretch mimics passive adduction. The person crosses the arm in front of the body, bringing the elbow of the affected arm toward the opposite shoulder. Have her place the other hand on the elbow, then pull in toward the opposite shoulder (Image 5). Make sure the elbow is on the same or a slightly higher level with the shoulder, not below it. Only a slight pull, not pain, should be felt in the shoulder. Rest a moment between stretches, and be sure to hold each stretch for the full 30 seconds. Repeat five times.

Image 5: This stretch mimics passive adduction
Injection
One or two corticosteroid injections given by a physician trained in orthopedic medicine are usually effective (a physician trained in non-surgical treatment of musculoskeletal pain). This injection should be followed by several days of rest and six weeks of rehabilitation. One or two injections of proliferant are effective in chronic cases where the tendon has been distended and weakened. The proliferant stimulates the build-up of strength in the tendon. The rehabilitation exercises outlined above should be used during this period.
References
[bg_collapse view=”button-orange” color=”#4a4949″ expand_text=”Show More” collapse_text=”Show Less” ]
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3084009/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4295680/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4246390/
- https://www.ncbi.nlm.nih.gov/pubmed/15160255
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4246390/
- https://www.sciencedirect.com/topics/neuroscience/infraspinatus-muscle
- https://socratic.org/questions/what-is-infraspinatus-tendonitis
- http://www.prioryclinic.com/library/article/infraspinatus_tendinitis
- https://www.p2sportscare.com/articles/upper-extremity/infraspinatus-strain/
- https://www.p2sportscare.com/articles/upper-extremity/infraspinatus-strain/
- https://www.cancertherapyadvisor.com/home/decision-support-in-medicine/shoulder-and-elbow/
[/bg_collapse]
