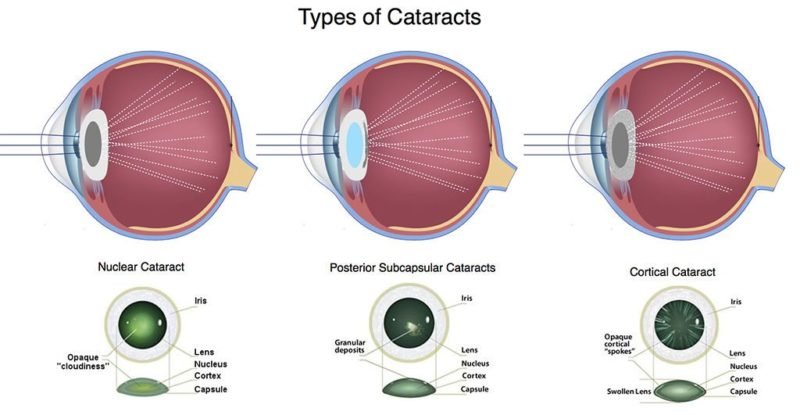
Posterior Subcapsular Cataracts/Cortical cataracts usually begin with either sharp limited clear fluid clefts, resulting in opaque spokes, or clear lamellar separations, resulting in cuneiform opacities. Cataracts is an eye condition in which the lens of the eye becomes cloudy. This causes vision to worsen, making it especially difficult to see fine details clearly. Some people’s vision is only slightly affected, whereas others might lose their eyesight very quickly. How it progresses will depend on things like the exact type of cataract. The word “cataract” comes from the Greek word for “waterfall” because in the past it was believed that the blurring was caused by a fluid in the eye.
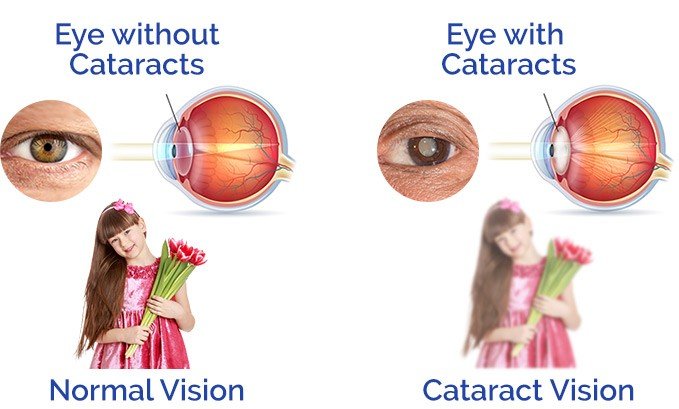
A cataract is a clouding of the lens in the eye which leads to a decrease in vision.[rx] Cataracts often develop slowly and can affect one or both eyes.[rx] Symptoms may include faded colors, blurry or double vision, halos around light, trouble with bright lights, and trouble seeing at night.[rx] This may result in trouble driving, reading, or recognizing faces.[rx] Poor vision caused by cataracts may also result in an increased risk of falling and depression.[rx] Cataracts cause half of all cases of blindness and 33% of visual impairment worldwide.[rx][rx]
Types of Cataracts
The type and progression of symptoms depends on various things, including what area of the lens is cloudy.
There are three main types of cataracts
-
Cortical cataracts – Apart from causing blurred vision, this type of cataract leads to problems with glare in particular, for instance when driving at night.
-
Posterior subcapsular cataracts – This type of cataract is more common in younger people and progresses relatively quickly.
-
Nuclear cataracts – These cataracts affect your ability to see things in the distance more than your ability to see nearby objects. Vision is sometimes affected only a little, and the condition progresses relatively slowly.
Although most cataracts are related to aging, there are other types of cataract
- Secondary cataract – Cataracts can form after surgery for other eye problems, such as glaucoma. Cataracts also can develop in people who have other health problems, such as diabetes. Cataracts are sometimes linked to steroid use.
- Traumatic cataract – Cataracts can develop after an eye injury, sometimes years later.
- Congenital cataract – Some babies are born with cataracts or develop them in childhood, often in both eyes. These cataracts may be so small that they do not affect vision. If they do, the lenses may need to be removed.
- Radiation cataract – Cataracts can develop after exposure to some types of radiation.
Main Effects of Different Types of Cataract
Nuclear cataract
-
Gradually reduced contrast
-
Reduced colour intensity
-
Reading often surprisingly good for level of Snellen acuity
-
Difficulty in seeing golf balls, car number plates, etc
-
Difficulty in recognising faces
Additional effects important in the developing world
-
Difficulty in working in fields at dusk
Cortical cataract
-
Light scatter from localised opacities and disruption of smooth light transmission
-
Problems with glare when driving
-
Difficulty reading
-
Sunlight uncomfortable in winter when sun low on horizon (northern and southern latitudes)
Additional effects important in the developing world
-
Difficulty in night driving
-
Compatible with daytime activities as the pigmented iris remains constricted
Subcapsular cataract
-
Visually disabling in good lighting—less trouble at low light levels when pupil is dilated
-
Difficulty in daytime driving
-
Difficulty in reading
Additional effects important in the developing world
-
Visually disabling as sunlight can be particularly bright
Etiological Types
Multiple factors responsible for developing cataracts include the following:
Congenital Cataract – Can be unilateral or bilateral – studies have documented a close association between congenital cataract and maternal nutrition, infections (rubella & German measles) and deficiency of oxygenation due to placental hemorrhage.
Age-related (Senile Cataract): Most common type of cataract
Traumatic Injury[rx][rx] – Most common cause of unilateral cataract in young adults
-
Perforating trauma
-
Blunt trauma: causing a characteristic flower-shaped opacity
-
Electric shock: a rare cause of cataract, causing diffuse milky-white opacification and multiple snowflakes like opacities, sometimes in a stellate subcapsular distribution
-
Ultraviolet radiation: if intense may rarely cause true exfoliation of the anterior lens capsule and cataract
-
Ionizing radiation: usage for ocular tumor treatment and in cardiological interventions may cause posterior subcapsular opacities
-
Chemical injuries: naphthalene, thallium, lactose, galactose
Systemic Diseases
-
Myotonic dystrophy
-
Atopic dermatitis
-
Neurofibromatosis type 2
Endocrine Diseases[rx]
-
Diabetes mellitus
-
Hypoparathyroidism
-
Cretinism
Primary Ocular Diseases
-
Chronic anterior uveitis – the most common cause of secondary cataract
-
Acute congestive angle closure – may cause small anterior grey- white subcapsular or capsular opacities, glaukomflecken
-
High myopia – may cause posterior subcapsular lens opacities and early-onset nuclear sclerosis, worsening the myopic refractive error
-
Hereditary fundus dystrophies – i.e, retinitis pigmentosa, Leber congenital amaurosis, gyrate atrophy and Stickler syndrome, may cause posterior and anterior subcapsular lens opacities
-
Poor Nutrition[rx] – a diet deficient in anti-oxidants and vitamins
-
Alcohol Abuse
-
Smoking
Causes of Cataracts
Developing cataracts is a normal part of growing older. Most people start to develop cataracts after the age of 65, but some people in their forties and fifties can also develop cataracts.
- Genetic factors – Genetically determined cataract is due to an anomaly in the chromosomal pattern of the individual. About one third of all congenital cataracts are hereditary.[rx] It may occur with or without microphthalmia, aniridia, anterior chamber developmental anomalies, retinal degenerations, other multisystem genetic disorders such as chromosome abnormalities, Lowe syndrome or neurofibromatosis type.[rx]
- Maternal and fetal factors – Malnutrition during pregnancy or in early infancy has been associated with non-familial zonular cataract. Maternal infections like rubella, toxoplasmosis, and cytomegalo-inclusion etc., are also associated with congenital cataracts.[rx]
- Gender – Women have a higher incidence and risk for most types of cataracts than men,[rx] probably due to lack of estrogen in post-menopausal years. An experimental study suggested the protective effects of estradiol or estrone treatment against cataractous eyes up to 25%, in the MNU-treated, ovariectomized rats.[rx]
- Race and ethnicity – African-Americans and Hispanic Americans seem to have nearly twice the risk of developing cataracts than Caucasians. This difference may be due to other medical illnesses, particularly diabetes, and due to lack of treatment.[rx]
- Ageing – Age-related (or senile) cataract is defined as cataract occurring in people >50 years of age, unrelated to known mechanical, chemical, or radiation trauma. It becomes progressively more severe and frequent in elderly[rx] and is responsible for 48% of world blindness.[rx]
- Diarrhea/dehydrational crisis – Minassian [rx] reported that one episode of severe diarrhea is 4.1 times more likely to cause cataract. The risk rose to 21% with two or more episodes of diarrhea and was still higher in those with history of both severe diarrhea and heatstroke. Harding[rx]
- Hypertension – Early clinical studies of cataract formation in diabetes mellitus noted a high prevalence of arterial hypertension.[17] Decreased lenticular ionic transport resulting from a specific decrease in Na+ K+ Adenosine Triphosphatase (ATPase) activity in the lens epithelium leads to cataract formation in the Nakano mouse.[18]
- Smoking – The role of smoking in cataractogenesis has been highlighted in various studies.[rx,rx,rx] These studies have shown 2-3 fold increased risk of cataract in smokers. The increase in smoking dose was associated with increasing severity of nuclear opacities. Aromatic compounds present in the inhaled smoke oxidatively modify lenticular components.[rx]
- Oxidative stress – oxygen-free radicals (Oxidants) – It is widely accepted that oxidative stress is a significant factor in the genesis of cataract, both in experimental animals[rx,rx] and in cultured lens models.[rx,rx] The oxidative processes rise with age in the human lens, and concentration of proteins found significantly higher in cataractous lenses.[rx]
- Metabolic – These cataracts occur due to endocrine disorders and biochemical abnormalities. Galactosemic and diabetic cataracts are common example of this kind of cataract.
- Galactosemia – Galactosemia is associated with inborn error of galactose metabolism, which can occur due to deficiency of galactose-1 phosphate uridyl-transferase (GPUT) and due to deficiency of galactokinase (GK). Development of bilateral cataract in the form of oil droplet central lens opacities is characteristic feature of galactosemia.[rx]
- Diabetes – Poor control of diabetes mellitus (DM) is linked to the formation of several systemic and ocular complications included vision loss.[rx] Evidently, direct in vivo and in vitro experimental studies suggest that diabetes is a cause of cataract. Uncontrolled DM results in hyperglycemia, which is associated in ocular tissues with non-enzymatic protein glycation,[rx] osmotic stress,[rx] and oxidative stress.[rx]
- Hypocalcemia – Cataractous changes may be associated with parathyroid tetany, which may occur due to atrophy or inadvertent removal (during thyroidectomy) of parathyroid glands. Multicolored crystals or small discreet white flacks of punctate opacities are formed in the sub-capsular region of lens, which seldom matures.[rx]
- Hypothyroidism – Cataract is not a common feature of hypothyroidism or cretinism; however, an association has been claimed,[rx] and the described opacities resemble those seen in hypoparathyroidism. Thyroidectomy without interference with the parathyroids has also been stated to cause cataract, usually a blue dot type.
- Error of copper metabolism – Inborn error of copper metabolism results in Wilson’s disease (hepatolenticular degeneration) may develop a characteristic opacity in the anterior capsular region brightly-colored sunflower pattern, green-colored, and has negligible effect on vision. The more commonly observed feature is ‘Kayser-Fleischer ring’ in the cornea.[rx,rx]
- Nutritional – Animal studies and in vitro investigations have shown that nutritional deficiencies of micronutrients are associated with cataract.
- Aldose reductase – (for reduction of sugars) is the basis for the formation of cataracts related to abnormalities in sugar metabolism.[rx,rx] Studies suggested that poor nutritional status of cataract patients accelerates protein insolubilization in the lens of most types of human and experimentally induced animal cataracts.[rx] Tryptophan deficiency-induced cataract has consistently been documented.[rx]
- Radiation – Cataracts can arise as an effect of exposure to various types of radiation. X-rays, one form of ionizing radiation, may damage the DNA of lens cells.[rx] Ultraviolet light, specifically UVB, has also been shown to cause cataracts, and some evidence indicates sunglasses worn at an early age can slow its development in later life.[rx] Microwaves, a type of nonionizing radiation, may cause harm by denaturing protective enzymes (e.g., glutathione peroxidase), by oxidizing protein thiol groups (causing protein aggregation), or by damaging lens cells via thermoelastic expansion.[rx]The protein coagulation caused by electric and heat injuries whitens the lens.[rx] This same process is what makes the clear albumen of an egg become white and opaque during cooking.
- Inadequate vitamin C- Low vitamin C intake and serum levels have been associated with greater cataract rates.[rx] However, use of supplements of vitamin C has not demonstrated benefit.[rx]
- Medications– Some medications, such as systemic, topical, or inhaled corticosteroids, may increase the risk of cataract development.[rx][rx] Corticosteroids most commonly cause posterior subcapsular cataracts.[rx] People with schizophrenia often have risk factors for lens opacities (such as diabetes, hypertension, and poor nutrition) but antipsychotic medications are unlikely to contribute to cataract formation.[rx] Miotics[rx] and triparanol may increase the risk.[rx] Corticosteroids and anticholinesterase inhibitors can cause both posterior and anterior subcapsular opacities respectively
- Trauma – having an eye injury can cause the injured eye to develop a cataract.
- Eye surgery – surgery for a retinal problem will likely lead to cataracts in the affected eye at some point in the future.
- Eye conditions – other eye conditions, such as retinitis pigmentosa, glaucoma or uveitis, may also cause cataracts.
- Having high myopia – (being very short sighted) may cause cataracts.
Symptoms of Cataracts
- Clouded, blurred or dim vision
- Increasing difficulty with vision at night
- Sensitivity to light and glare
- Need for brighter light for reading and other activities
- Seeing “halos” around lights
- Seeing double (when you see two images instead of one)
- Being extra sensitive to light
- Having trouble seeing well at night, or needing more light when you read
- Seeing bright colors as faded or yellow instead
- Frequent changes in eyeglass or contact lens prescription
- Fading or yellowing of colors
- Double vision in a single eye
- People with nuclear sclerotic or brunescent cataracts often notice a reduction of vision.
- Nuclear cataracts typically cause greater impairment of distance vision than of near vision.
- Those with posterior subcapsular cataracts usually complain of glare as their major symptom.
- The severity of cataract formation, assuming no other eye disease is present, is judged primarily by a visual acuity test. Other symptoms include frequent changes of glasses and colored halos due to hydration of lens.
Diagnosis of Cataracts
History
The patient may present with one of the following symptoms:
-
Decrease or blurring in vision – gradual and painless; unilateral or bilateral depending upon the eye being affected without and at mature stages even with glasses
-
Diplopia or polyopia – mostly uniocular but can be binocular- this is due to multiple refractions through clear areas between the opacities
-
Colored halos around the light – Rainbow halos; possibly due to the collection of water drops between layers of lens fibers acting as a prism splitting light into its seven colors
-
Sensitivity to glare – especially headlights of automobiles and sunlight
-
Increased frequency to change refractive glasses – as the cataract matures, a person may visit his ophthalmologist more often for refraction
-
Disturbance in color vision – fading or yellowing of objects
Physical Findings
Following findings can be noticed during a thorough ophthalmic examination depending upon the part of the lens involved:
Visual Acuity
-
Decreased unilaterally or bilaterally depending upon the affected eye
Cortical Cataract
-
Wedge-shaped opacity with clear areas of lens matter mostly present at the periphery (Incipient cortical cataract)
-
Well-developed wedge-shaped opacity (Progressive cortical cataract)
-
Advanced opacity with a greyish lens, clear cortex, and an iris shadow (Immature cortical cataract)
-
Findings of the immature stage but with a swollen lens due to the accumulation of fluid making anterior chamber shallow (Intumescent cortical cataract)
-
The entire opaque cortex with the absence of iris shadow (Mature cortical cataract)
-
Milky fluid bag with lens nucleus present at the bottom due to liquefaction of the cortex without an iris shadow and a shallow anterior chamber (Hypermature cortical cataract)
Nuclear Cataract
-
Dark brown or black lens with an iris shadow
-
No fundal view due to dark opacity in the center against a red glow
-
No fourth Purkinje image
Systemic Diseases
-
Diabetes mellitus – classic snowflake cortical opacities
-
Myotonic dystrophy – Christmas tree cortical cataract which later evolves into wedge-shaped cortical and subcapsular opacities resembling a star-like in conformation
-
Atopic Dermatitis – characteristic shield-like dense anterior subcapsular plaques
-
Neurofibromatosis type 2 – mixed opacities; can be subcapsular, capsular or cortical
Evaluation
Cataracts can be evaluated by a number of steps as follows:
History
-
The chief complaint of the patient, i.e., a decrease of vision
-
Past ophthalmic history
-
Any systemic disease causing or aggravating the symptoms
Comprehensive ophthalmic examination
-
Visual acuity – can be assessed by Snellen chart to identify the severity of the disease and limitations in routine activities of life
-
Refraction – Important factor to plan management
-
Cover test – poor vision caused by cataract can be a reason for a divergent squint
-
Slit Lamp Examination
-
Pupillary responses – to check the shape of the pupil, afferent and efferent pathways and relative afferent pupillary defect
-
Adenexal examination – a thorough examination is needed to exclude any adnexal pathology, i.e., dacryocystitis, blepharitis, chronic conjunctivitis, lagophthalmos, ectropion, entropion, and tear film abnormalities – these conditions may predispose to endophthalmitis, so their diagnosis and optimization are necessary to treat cataract
-
Cornea – important to asses whether cornea will able to handle operative trauma – arcus senilis is an important finding because it can obstruct the operative field clarity
-
Anterior Chamber – a shallow anterior chamber can make cataract surgery extremely difficult
-
Lens – part of the lens involved can be an important factor to plan our surgical technique – nuclear cataract is harder while cortical cataract is softer in consistency
-
Fundus Examination – any pathology in the fundus, i.e., age-related macular degeneration can be an important factor to determine visual outcome after surgery that is why a thorough fundal examination is critical
Investigations
The following investigations can help diagnose and plan the management of the disease:
-
Intraocular pressure – to rule out glaucoma
-
Dark Room Tests – direct and indirect ophthalmoscopy
-
Fundoscopy – to rule out any vitreous or retinal pathology
-
Biometry – for intraocular lens (IOL) placement during surgery
-
Peripheral Retinal Assessment – testing the projection of light in all quadrants
-
Macular function test – like cardboard test (two-point discrimination), Maddox rod test, the laser interferometry, foveal electroretinogram, photo stress test
-
Ultrasound scan – B-scan is advised to see retinal detachment or any vitreous pathology
-
Systemic diseases – Blood glucose levels, electrocardiography, echocardiography, ultrasonography
-
Baseline tests – Complete blood count, liver function test, renal function test, bleeding profile, Hep B & C screening, chest X-ray
- Dilated eye exam – Drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of damage and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
- Tonometry – An instrument measures the pressure inside the eye. Numbing drops may be applied to your eye for this test.
- Visual acuity test – A visual acuity test uses an eye chart to measure how well you can read a series of letters. Your eyes are tested one at a time, while the other eye is covered. Using a chart or a viewing device with progressively smaller letters, your eye doctor determines if you have 20/20 vision or if your vision shows signs of impairment.
- Slit-lamp examination – A slit lamp allows your eye doctor to see the structures at the front of your eye under magnification. The microscope is called a slit lamp because it uses an intense line of light, a slit, to illuminate your cornea, iris, lens, and the space between your iris and cornea. The slit allows your doctor to view these structures in small sections, which makes it easier to detect any tiny abnormalities.
- Retinal exam – To prepare for a retinal exam, your eye doctor puts drops in your eyes to open your pupils wide (dilate). This makes it easier to examine the back of your eyes (retina). Using a slit lamp or a special device called an ophthalmoscope, your eye doctor can examine your lens for signs of a cataract.
Treatment / Management
The treatment choice depends upon the degree of opacity sufficient enough to cause difficulty in performing essential daily activities. Following treatment modalities are available:
-
Medical – If visual acuity is 6/24 or better, pupillary dilatation with 2.5% phenylephrine or refractive glasses are enough to carry on routine activities, and surgery is not required. Cyclopentolate and atropine can also be useful. Recently, there are also cataracts drops under trial which can dissolve cataract.
-
Surgery – If visual acuity is worse than 6/24 or there is a medical indication (phacolytic glaucoma, phacomorphic glaucoma, retinal detachment) in which a cataract is adversely affecting the health of the eye, surgery is always needed. Irrigation and aspiration of the lens, Irrigation and aspiration of the lens with IOL implantation, Irrigation aspiration of the lens with IOL, anterior vitrectomy and primary posterior capsulotomy
- Congenital Cataract – No treatment is necessary if visual acuity is more than 6/24 and a patient can carry out their normal routine activities. Refractive glasses can be advised for the blurring of vision or diplopia. If visual acuity falls below 6/24, surgery is needed and the surgeon can opt one of the following surgical procedures depending upon patients complaints and severity of the disease.[rx]
-
Senile Cataract – Treatment options are the following[rx][rx]
-
Medical: No medical treatment is effective once the cataract has become mature.
-
Surgical: Mature cataract has a very hard nucleus, and one of the following methods are used to extract lens:
-
Extracapsular cataract extraction: a procedure of choice
-
Intracapsular cataract extraction: an old technique not used frequently due to complications
-
Phaco-emulsification: a modification of ECCE with less astigmatism and early visual recovery
-
Laser phacolysis: a recent advancement under trial
-
-
-
Management of general conditions before surgery: There are many general health conditions which require optimization before surgery for the better results.
-
Diabetes mellitus
-
Hypertension
-
Myocardial Infarction
-
Angina
-
Respiratory Infection
-
Stroke
-
Leg ulcer
-
Viral hepatitis
-
AIDS
-
Epilepsy
-
Parkinson disease
-
Rheumatoid arthritis
-
- Aldose-Reductase Inhibitors – Aldose reductase inhibitors (ARI) comprise a variety of structurally different compounds like plant extracts, animal tissues or specific small molecules. In diabetic rats, plant flavonids, such as quercitrin or the isoflavone genistein, have delayed diabetic cataract formation [rx–rx]. Examples of natural products with known AR inhibitory activity are extracts from indigenous plants like Ocimum sanctum, Withania somnifera, Curcuma longa, and Azadirachta indica or the Indian herbal Diabecon [rx, rx]. Levels of polyol in the lenses of rats have been reduced by injection of intrinsic ARI containing extracts from human kidney and bovine lenses [rx]. Nonsteroidal anti-inflammatory drugs, such as sulindac [rx, rx], aspirin [rx, rx] or naproxen [rx] have been reported to delay cataract in diabetic rats through a weak AR inhibitory activity.
- Pyruvate – an endogenous antioxidant, has recently gained attention for its inhibitory effect on diabetic cataract formation by reducing sorbitol formation and lipid peroxidation in the lens [rx]. A study performed by Varma et al. showed that the incidence of cataract in diabetic rats was lower in the pyruvate-treated group than in the untreated control group [rx].
- Nepafenac – a topical NSAID indicated for the prevention and treatment of anterior segment pain and inflammation after cataract surgery, has been used recently in clinical trials to test its efficacy in reducing the incidence of macular edema after cataract surgery. The active ingredient is a prodrug that rapidly penetrates the cornea to form the active metabolite, amfenac, by intraocular hydrolases particularly in the retina, ciliary body epithelium and choroid [rx].
Surgery
There are two generic terms for cataract extraction—intracapsular and extracapsular.
- Intracapsular extraction – involves removing the whole lens still within its intact capsule. This technique is no longer used in the developed world (except in rare specific circumstances) as the visual results are generally poorer and the operative and postoperative complications greater than with the alternative. It remains common in the developing world, however, because it requires less costly and sophisticated instruments, there is less dependency on back-up services and a reliable electricity supply, and it can be performed after a minimum of training.
- Extracapsular extraction – involves removing the lens from its capsule, which is retained within the eye and acts as a barrier between the anterior and posterior segments as well as forming the most usual site for replacement lens implantation. In manual extracapsular extraction the nucleus of the lens is removed en bloc, and therefore requires a relatively large incision.
Phacoemulsification – is the most widely used cataract surgery in the developed world.[rx][rx] This procedure uses ultrasonic energy to emulsify the cataract lens. Phacoemulsification typically comprises six steps:
- Anaesthetic – The eye is numbed with either a subtenon injection around the eye or topical anesthetic eye drops. The former also provides paralysis of the eye muscles.
- Corneal incision – Two cuts are made at the margin of the clear cornea to allow insertion of instruments into the eye.
- Capsulorhexis – A needle or small pair of forceps is used to create a circular hole in the capsule in which the lens sits.
- Phacoemulsification – A handheld ultrasonic probe is used to break up and emulsify the lens into liquid using the energy of ultrasound waves. The resulting ’emulsion’ is sucked away.
- Irrigation and aspiration – The cortex, which is the soft outer layer of the cataract, is aspirated or sucked away. Fluid removed is continually replaced with a saline solution to prevent collapse of the structure of the anterior chamber (the front part of the eye).
- Lens insertion – A plastic, foldable lens is inserted into the capsular bag that formerly contained the natural lens. Some surgeons also inject an antibiotic into the eye to reduce the risk of infection. The final step is to inject salt water into the corneal wounds to cause the area to swell and seal the incision.
- Small-incision cataract surgery – involves making an incision in the side of the cornea (the clear outer covering of the eye) and inserting a tiny probe into the eye. The probe emits ultrasound waves that soften and break up the lens so it can be suctioned out. This process is called phacoemulsification.
- Extracapsular surgery – requires a somewhat larger incision in the cornea so that the lens core can be removed in one piece. The natural lens is replaced by a clear plastic lens called an intraocular lens (IOL). When implanting an IOL is not possible because of other eye problems, contact lenses and, in some cases, eyeglasses may be an option for vision correction.
Complications
Cataract cause multiple complications discussed as follows:
Congenital Cataract: These can be disease related or surgery related[rx]
-
Disease-related complications – corneal ulcer, corneal perforation (acquired anterior capsular cataract), blindness
-
Surgery-related complications – uveitis, posterior capsular thickening, aphakia, after cataract, growth-related refractive changes, glaucoma, retinal detachment
-
Disease-related complications – acute congestive glaucoma (Intumescent stage), phacolytic glaucoma, iritis, subluxation of the lens, secondary glaucoma(hyper mature stage), blindness
-
Surgery-related complications – these are classified as follows:
-
Post Surgery[rx][rx] – iris prolapse, delayed anterior chamber formation, infections like endophthalmitis or panophthalmitis, striate keratitis, malpositioning of IOL, pseudophakic glaucoma, cystoid macular edema, dysphotopsia, ptosis, retinal detachment, posterior capsular thickening, and opacifications
-
During Surgery – posterior capsular rupture, hyphaema, expulsive hemorrhage, corneal burn, nucleus drop in vitreous
Prevention
- Have regular eye examinations – Eye examinations can help detect cataracts and other eye problems at their earliest stages. Ask your doctor how often you should have an eye examination.
- Quit smoking – Ask your doctor for suggestions about how to stop smoking. Medications, counseling and other strategies are available to help you.
- Manage other health problems – Follow your treatment plan if you have diabetes or other medical conditions that can increase your risk of cataracts.
- Choose a healthy diet that includes plenty of fruits and vegetables. Adding a variety of colorful fruits and vegetables to your diet ensures that you’re getting many vitamins and nutrients. Fruits and vegetables have many antioxidants, which help maintain the health of your eyes.
- Wear sunglasses – Ultraviolet light from the sun may contribute to the development of cataracts. Wear sunglasses that block ultraviolet B (UVB) rays when you’re outdoors.
- Reduce alcohol use – Excessive alcohol use can increase the risk of cataracts.
- Nutrition: Healthy food reduces the risk of disease, including eye problems. A healthy diet has plenty of fruits, vegetables, whole grains, unrefined carbohydrates, good quality fats, such as avocado, olive oil, and omega oils, and either plant-sourced proteins or lean, animal-sourced proteins.
- Obesity and diabetes: Obesity significantly raises the risk of developing type 2 diabetes, a cataract risk factor. Maintaining a healthy weight and keeping diabetes under control will help reduce the risk.Other factors that can help to protect against cataracts are:
- Wearing sunglasses that block UV radiation when in sunlight
- Get at least 7 hours of good quality, continuous sleep every night
References
[bg_collapse view=”button-orange” color=”#4a4949″ expand_text=”Show More” collapse_text=”Show Less” ]
- https://www.ncbi.nlm.nih.gov/books/NBK539699/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3178670/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4097885/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3061107/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2684074/
- https://www.ncbi.nlm.nih.gov/books/NBK390302/
- https://www.ncbi.nlm.nih.gov/books/NBK481726/
- https://www.ncbi.nlm.nih.gov/books/NBK333487/
- https://www.ncbi.nlm.nih.gov/books/NBK263908/
- https://www.ncbi.nlm.nih.gov/books/NBK476171/
- https://www.ncbi.nlm.nih.gov/books/NBK390312/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6139750/
- https://www.ncbi.nlm.nih.gov/books/NBK536577/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4069779/
- https://nei.nih.gov/health/cataract/cataract_facts
- https://nei.nih.gov/health/cataract
- https://en.wikipedia.org/wiki/Cataract
- https://www.mayoclinic.org/diseases-conditions/cataracts/diagnosis-treatment/drc-20353795
- https://www.medicalnewstoday.com/articles/157510.php
- http://www.bausch.com/your-eye-concerns/diseases-and-disorders/cataracts
- https://www.aao.org/eye-health/diseases/what-are-cataracts
- https://www.preventblindness.org/cataract
- https://www.nhs.uk/conditions/cataracts/
- https://www.sightsavers.org/protecting-sight/what-are-cataracts/
- https://www.aao.org/eye-health/diseases/what-are-cataracts
- https://www.aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions/cataract
[/bg_collapse]