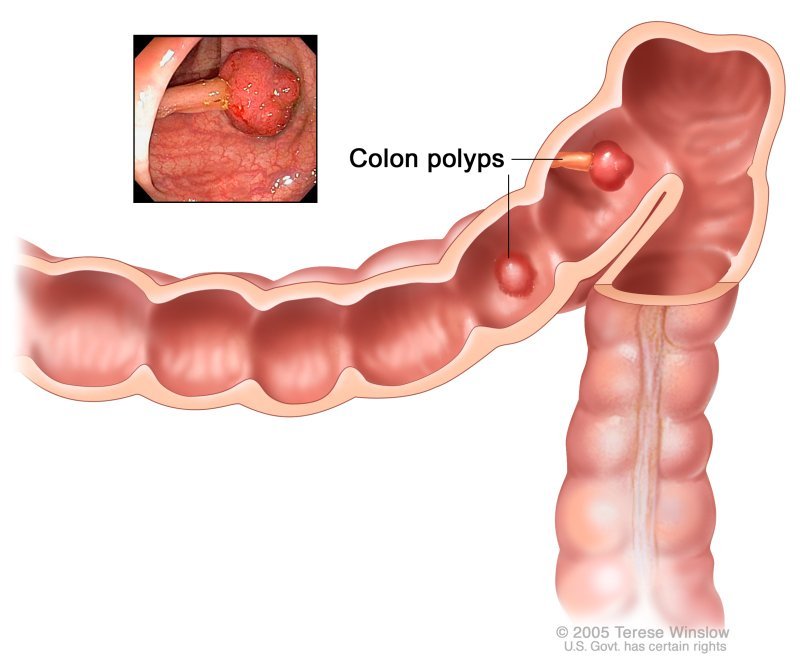
Colon polyps also known as colorectal polyps are their macroscopic appearance as sessile (flat, arising directly from the mucosal layer) or pedunculated (extending from the mucosa through a fibrovascular stalk) growths on the lining of your colon and rectum. You can have more than one colon polyp. Colon polyps are protrusions occurring in the colon lumen most commonly sporadic or as part of other syndromes. Polyps are classified as diminutive if 5 mm in diameter or less, small if 6 to 9 mm, or large if they are 1 cm in diameter or more. Polyps can be depressed, flat, sessile or pedunculated. Few polyps arise from submucosa including lipomas, carcinoids, or lymphoid aggregates. Most commonly, however, they result from the mucosa, and they can be adenomatous, serrated, or non-neoplastic.
Types of colonic polyps
Polyps in the colon can vary in size and number. There are 5 types of colon polyps
- Hyperplastic polyps – are harmless and don’t develop into cancer.
- Adenomatous polyps – are the most common. Although most will never develop into cancer, they do have the potential to become colon cancer.
- Malignant polyps – are polyps that are noted under microscopic examination to have cancer cells in them.
- Adenomas – Two-thirds of colon polyps are the precancerous type, called adenomas. It can take seven to 10 or more years for an adenoma to evolve into cancer—if it ever does. Overall, only 5% of adenomas progress to cancer, but your individual risk is hard to predict. Doctors remove all the adenomas they find
- Sessile serrated polyps – Once thought harmless, this type of adenoma is now known to be risky. These are also removed.
Causes of Colon Polyps
Hereditary disorders that cause colon polyps include:
- Lynch syndrome – also called hereditary nonpolyposis colorectal cancer. People with Lynch syndrome tend to develop relatively few colon polyps, but those polyps can quickly become malignant. Lynch syndrome is the most common form of inherited colon cancer and is also associated with tumors in the breast, stomach, small intestine, urinary tract, and ovaries.
- Familial adenomatous polyposis (FAP) – a rare disorder that causes hundreds or even thousands of polyps to develop in the lining of your colon beginning during your teenage years. If the polyps aren’t treated, your risk of developing colon cancer is nearly 100 percent, usually before age 40. Genetic testing can help determine your risk of FAP.
- MYH-associated polyposis (MAP) – A problem with the MYH gene causes many polyps to grow or colon cancer to happen at a young age.
- Peutz-Jeghers syndrome – The condition starts with freckles that show up all over the body. It also causes colon polyps that can become cancer.
- Serrated polyposis syndrome – This causes a specific type of polyp, serrated adenomatous polyps, to grow in the upper part of the colon. They can turn into colon cancer.
- Gardner’s syndrome – a variant of FAP that causes polyps to develop throughout your colon and small intestine. You may also develop noncancerous tumors in other parts of your body, including your skin, bones and abdomen.
- MYH-associated polyposis (MAP) – a condition similar to FAP that is caused by mutations in the MYH gene. People with MAP often develop multiple adenomatous polyps and colon cancer at a young age. Genetic testing can help determine your risk of MAP.
- Peutz-Jeghers syndrome – a condition that usually begins with freckles developing all over the body, including the lips, gums, and feet. Then noncancerous polyps develop throughout the intestines. These polyps may become malignant, so people with this condition have an increased risk of colon cancer.
- Serrated polyposis syndrome – a condition that leads to multiple serrated adenomatous polyps in the upper part of the colon. These polyps may become malignant.
Symptoms of Colon Polyps
Most people with colon polyps don’t have symptoms. You can’t tell that you have polyps because you feel well. When colon polyps do cause symptoms, you may
But some people with colon polyps experience:
- Rectal bleeding – This can be a sign of colon polyps or cancer or other conditions, such as hemorrhoids or minor tears in your anus.
- Change in stool color – Blood can show up as red streaks in your stool or make stool appear black. A change in color may also be caused by foods, medications, and supplements.
- Change in bowel habits – Constipation or diarrhea that lasts longer than a week may indicate the presence of a large colon polyp. But a number of other conditions can also cause changes in bowel habits.
- Pain – A large colon polyp can partially obstruct your bowel, leading to crampy abdominal pain.
- Iron deficiency anemia – Bleeding from polyps can occur slowly over time, without visible blood in your stool. Chronic bleeding robs your body of the iron needed to produce the substance that allows red blood cells to carry oxygen to your body (hemoglobin). The result is iron-deficiency anemia, which can make you feel tired and short of breath.
- Red blood mixed in with or on the surface of the stool
- Black stools if the polyp is bleeding substantially and is located in the proximal colon (cecum and ascending colon)
- Weakness, light-headedness, fainting, pale skin, and rapid heart rate due to iron deficiency anemia
- The presence of invisible (occult) blood in stool that is tested when screening for colon cancer at visits to a doctor’s office (Because of the tendency of polyps to bleed slowly, intermittently and in small amounts, occult blood testing of stool often is used to screen for colon cancer.)
- Rarely diarrhea when large villous polyps secrete fluid into the intestine
- Rarely constipation if the polyp is very large and obstructs the colon
- Rarely intussusception, a condition in which a polyp drags the portion of the colon to which it is attached into the more distal colon (i.e., telescopes into the more distal colon) and leads to obstruction of the colon. This can cause all of the signs and symptoms of intestinal obstruction including abdominal pain and distention, nausea and vomiting.
- Have bleeding from your rectum. You might notice blood on your underwear or on toilet paper after you’ve had a bowel movement.
- Have blood in your stool. Blood can make stool look black or can show up as red streaks in your stool.
- Feel tired because you have anemia and not enough iron in your body. Bleeding from colon polyps can lead to anemia and a lack of iron.
Many other health problems can also cause these symptoms. However, if you have bleeding from your rectum or blood in your stool, contact your doctor right away.
Diagnosis of Colon Polyps
Doctors can find colon polyps only by using certain tests or procedures, such as a colonoscopy or imaging study. Your doctor may first take a medical and family history and perform a physical exam to help decide which test or procedure is best for you.
For example, your doctor may ask if you have any symptoms. He or she may also ask if you have a family history of colon polyps or colorectal cancer. After taking a medical and family history, your doctor may perform a physical exam.
Tests and procedures
- Flexible sigmoidoscopy – For a flexible sigmoidoscopy, a trained medical professional uses a sigmoidoscope—a flexible, narrow tube with a light and tiny camera on one end—to look inside your rectum and lower colon. Flexible sigmoidoscopy can show irritated or swollen tissue, ulcers, polyps, and cancer.
- Colonoscopy – During a colonoscopy, a trained medical professional uses a long, flexible, narrow tube with a light and tiny camera on one end, called a colonoscope, to look inside your rectum and colon. Colonoscopy can show irritated and swollen tissue, ulcers, polyps, and cancer. The most sensitive test for colorectal polyps and cancer. If polyps are found, your doctor may remove them immediately or take tissue samples (biopsies) for analysis.
- Virtual colonoscopy – Virtual colonoscopy uses x-rays and a computer to create images of your rectum and colon from outside the body. Virtual colonoscopy can show ulcers, polyps, and cancer. Doctors can’t remove polyps during virtual colonoscopy.
- Lower gastrointestinal series – For a lower gastrointestinal (GI) series, a doctor uses x-rays and a chalky liquid called barium to view your large intestine. The barium will make your large intestine easier to see on an x-ray. A lower GI series is also called a barium enema.
- Virtual colonoscopy – a minimally invasive test that uses a CT scan to view your colon. Virtual colonoscopy requires the same bowel preparation as a colonoscopy. If a polyp is found, you’ll need a colonoscopy to have it removed.
- CT colonography – Also known as a virtual colonoscopy, this uses X-rays and a computer to take pictures of your colon from outside your body. Your doctor can’t take polyps out during this test. If they spot any, you’ll need to have a regular colonoscopy. You’re awake for this test, but you’ll still need to do a special diet to clear out your bowel beforehand.
- Flexible sigmoidoscopy – in which a slender, lighted tube is inserted in your rectum to examine it and the last third of your colon (sigmoid) and rectum. If a polyp is found, you’ll need a colonoscopy to have it removed.
- Stool-based tests – This type of test works by checking for the presence of blood in the stool or assessing your stool DNA. If your stool test is positive you will need a colonoscopy.
- Fecal occult blood testing – (FOBT) may indicate bleeding from a colonic polyp. A positive FOBT due to bleeding from a polyp correlates to the polyp size and proximity to the rectum. Most small polyps will fail to result in a positive FOBT, although the test has a higher sensitivity for larger polyps and for carcinomas. For this reason, FOBT is a part of the screening algorithm for the early detection of colon cancer, despite its poor sensitivity for polyps.
- Fecal immunochemical testing – (FIT or iFOBT) is a newer, more sensitive screening method than the traditional FOBT. It utilizes specific antibodies to the globin component of the hemoglobin. A recent study compared FIT against colonoscopy as a screening tool for both colorectal cancer and adenomas [rx].
- Colonoscopic spectroscopy – using near-infrared autofluorescence (NIR AF) was recently proposed as an adjunct for in vivo diagnosis of colonic ‘pre-cancer and cancer during clinical colonoscopic screening. This method was found to have a sensitivity and specificity of approximately 80% and 90%, respectively, for the classification of benign, pre-cancer lesions and cancer in the colon [rx]. This method, although promising, is still experimental and is not routinely used in clinical practice.
- Narrow-band imaging – (NBI) is another new endoscopic imaging technique that highlights surface structures and superficial mucosal capillaries during colonoscopy. Even though disagreement exists regarding its effectiveness in increasing the colonoscopic view’s sensitivity, it has recently been shown to have a high sensitivity and specificity for differentiating neoplastic and non-neoplastic polyps [rx, rx]. This modality has also not entered routine clinical practice.
- Computed tomographic colonography – (also called ‘CT colonography’ or ‘virtual colonoscopy’) is another screening modality, which is suggested for patients who refuse colonoscopy. This modality uses computed tomography of an air-distended prepared colon. With an optimal colon preparation and an experienced radiologist reading the images, some reports indicate that the sensitivity of CT colonography for detecting polyps larger than 5 mm (which are believed to be clinically significant) exceeds 90% [rx, rx]
- Magnetic resonance colonography – (MRC) is another diagnostic modality that is currently being evaluated. The rationale for using MRC is based on the relatively high radiation exposure during CT colonography [rx]. A recent small-scale study has demonstrated a low sensitivity (despite a high specificity) for detecting large (>10 mm) polyps using MRC [rx]. Therefore, the evidence does not support MRC as a standard diagnostic modality for detecting colorectal polyps and this modality is not routinely used in clinical practice.
- Capsule endoscopy – is a diagnostic modality that was originally developed to diagnose and evaluate small bowel lesions. Since the capsule passes through the prepared colon after traversing the ileocecal valve and continues to transmit images, it can also detect colonic lesions. A large cohort with suspected colonic lesions underwent a capsule endoscopy with a dual camera capsule designed especially to evaluate the colon (PILLcam colon) and, immediately afterward, had a colonoscopy. The sensitivity and specificity of the capsule endoscopy were shown to be inferior to colonoscopy [rx].
- Fecal DNA and antigen testing – is another futuristic modality expected to yield results within the next few decades [rx]. Several technical advances have recently been seen to increase its accuracy, including the use of a DNA preservative buffer with stool collection, DNA amplification methods, and automated assays of several DNA markers [rx]. The stool was analyzed with an automated multi-target stool DNA assay to measure β-actin, mutant KRAS, aberrantly methylated BMP3 and NDRG4, and fecal hemoglobin.
- Stool DNA analysis – identified individuals with colorectal cancer with 98% sensitivity and 90% specificity. Its sensitivity in respect of advanced adenomas was 57% and for high-grade dysplasia, it was 83% [30]. In the future, should this modality prove to have even a higher positive predictive value for detecting adenoma or carcinoma, it might obviate the need for any invasive screening tests.
Second examination
- If no polyps are found on the first examination it is recommended that a second examination should be done 10 years later.
- If the only polyps that are found are hyperplastic polyps, and they are limited to the rectum and sigmoid colon and they are all less than one centimeter in size, a second examination is recommended in 10 years.
- If one or two tubular adenomas are found and they are less than one centimeter in size, a second examination is recommended in five years through a longer interval may be reasonable as well.
- If three to ten adenomas are found, it is recommended that a second examination be done in three years.
- If more than ten adenomas are found, it is recommended that a second examination be done in three years or less.
- If one or more tubular adenomas are found that are greater than one centimeter in size, a second examination is recommended in three years.
- If one or more adenomas are found of any size and their histology is villous, a second examination is recommended in three years.
- If one or more adenomas are found and any show high-grade dysplasia, a second examination is recommended in three years.
- If serrated polyps are found, recommendations are less secure because much less information is available about the future risk of polyps and cancers. Concerns are greater (and the interval to the next examination should be shorter) if the polyps are proximal (in the ascending colon), are larger (more than one centimeter in size), and particularly if they show dysplasia.
Treatment for Colon Polyps
Doctors treat colon polyps by removing them.
In most cases, doctors use special tools during a colonoscopy or flexible sigmoidoscopy to remove colon polyps. After doctors remove the polyp, they send it for testing to check for cancer. A pathologist will review the test results and send a report to your doctor. Doctors can remove almost all polyps without surgery.
If you have colon polyps, your doctor will ask you to get tested regularly in the future because you have a higher chance of developing more polyps.
Your doctor is likely to remove all polyps discovered during a bowel examination.
- Eat less meat – Eat a healthy diet, with minimal red meat—especially processed or cured meats. Studies suggest that people with meat-rich diets tend to have higher rates of colon cancer.
- antioxidants
–Several associations have been explored for antioxidants including selenium, beta carotene, and vitamins A, C, and E. Most of the studies that have been done do not support a role for these agents in preventing polyps or in preventing colon cancer. A limited amount of support is available for the use of selenium to prevent polyps, but selenium is not recommended for use outside of experimental trials. - Supplemental dietary calcium – has been demonstrated in one study to prevent the formation of polyps. The benefit was seen with supplementation of 1200 mg of calcium per day. There is some concern about using calcium since higher dietary and supplemental levels are associated with an increase in vascular disease. The intake of calcium that was studied was higher than the recommended intake of calcium, 800 mg per day.
- NSAIDs – The best support for a treatment to prevent polyps is with nonsteroidal anti-inflammatory drugs (NSAIDs), a class of drugs that includes aspirin, ibuprofen (Motrin, Advil), celecoxib (Celebrex), and many others. Aspirin has been shown in several studies to reduce the formation of polyps by 30% to 50%. The effect is likely to occur with higher doses of aspirin (more than the 81-325 mg that is recommended for cardiovascular disease prevention), and there is concern about aspirin’s side effect of gastrointestinal bleeding at these doses.
- Celecoxib (Celebrex), a “COX-2 selective NSAID” – or Cox-2 inhibitor has been shown to reduce colon polyps 30% to 50% as well, but there is a lingering concern about the possible cardiovascular side effects that may be seen with most NSAIDs (though the data supporting this side effect is conflicting). It may be used in patients with genetic polyposis syndromes who choose not to have their colons removed. Celecoxib might be considered in patients with a low risk for cardiovascular disease who develop adenomatous polyps frequently.
- Sulindac (Clinoril) – a “non-selective NSAID” has been shown to prevent polyps in patients with sporadic adenoma as well as genetic syndromes. As with celecoxib, there is concern about cardiovascular side effects and gastrointestinal ulceration and bleeding.
- Aspirin – Taking a low dose of aspirin every day for a long period of time may help prevent polyps from developing into colorectal cancer in some people. However, taking aspirin daily may cause side effects such as bleeding in your stomach or intestines. Talk with your doctor before you start taking aspirin daily.
Some types of colon polyp are far likelier to become malignant than are others. But a doctor who specializes in analyzing tissue samples (pathologist) usually must examine polyp tissue under a microscope to determine whether it’s potentially cancerous.
Surgery
- Removal with forceps or a wire loop (polypectomy) – If a polyp is larger than 0.4 inches (about 1 centimeter), a liquid may be injected under it to lift and isolate the polyp from surrounding tissue so that it can be removed.
- Minimally invasive surgery – Polyps that are too large or that can’t be removed safely during screening are usually removed laparoscopically, which is performed by inserting an instrument called a laparoscope into the bowel.
- Colon and rectum removal – If you have a rare inherited syndrome, such as FAP, you may need surgery to remove your colon and rectum (total proctocolectomy).
- Laparoscopy – During a laparoscopy, the doctor will make a small incision into the abdomen or pelvis and insert an instrument called a laparoscope into the bowel. They use this technique to remove polyps that are too large or cannot be removed safely by colonoscopy.
- Removing the colon and rectum – This procedure, known as a total proctocolectomy, is only necessary when a person has a severe condition or cancer. Doctors recommend this option for those with rare inherited conditions, such as familial adenomatous polyposis (FAP). FAP is an inherited condition that causes cancer of the colon and rectum, and polyp removal may prevent cancer from developing.
Seek Care Right Away
Call your doctor right away if you have any of the following symptoms after he or she removes a colon polyp:
- severe pain in your abdomen
- fever
- bloody bowel movements that do not get better
- bleeding from your anus that does not stop
- dizziness
- weakness
How can I prevent colon polyps?
Researchers don’t know a sure way to prevent colon polyps. However, you can take steps to lower your chances of developing colon polyps.
Eating, diet, and nutrition
Eating, diet, and nutrition changes—such as eating less red meat and more fruits and vegetables—may lower your chances of developing colon polyps.
You can make the following healthy lifestyle choices to help lower your chances of developing colon polyps:
- get regular physical activity
- don’t smoke cigarettes, and if you do smoke, quit
- avoid drinking alcohol
- lose weight if you’re overweight
- Being physically active and losing weight if you’re overweight may lower your chances of developing colon polyps.
How Can I Prevent Colon Polyps?
Healthy habits can lower your odds of having colon polyps. For example, you should:
- Eat a diet with lots of fruits, vegetables, and fiber-rich foods like beans, lentils, peas, and high-fiber cereal.
- Lose weight if you’re overweight.
- Limit red meat, processed meats, and foods that are high in fat.
- Talk to your doctor about whether calcium and vitamin D supplements are right for you. Some studies suggest they could lower your odds of colon cancer, but others don’t.
- If you have a family history of colon polyps, ask your doctor if you should get genetic counseling and when you should start screening for polyps.
- Talk to your doctor about taking aspirin regularly. There is some evidence that aspirin has a preventive effect against colon cancer.
REferences
[bg_collapse view=”button-orange” color=”#4a4949″ expand_text=”Show More” collapse_text=”Show Less” ]
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6878826/
- https://www.ncbi.nlm.nih.gov/books/NBK279198/
- https://www.ncbi.nlm.nih.gov/books/NBK1266/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5736948/
- https://www.ncbi.nlm.nih.gov/books/NBK470380/
- https://www.ncbi.nlm.nih.gov/books/NBK538233/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6878827/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6878826/
- https://www.ncbi.nlm.nih.gov/books/NBK51310/
- https://www.ncbi.nlm.nih.gov/books/NBK559064/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1069054/
- https://www.ncbi.nlm.nih.gov/books/NBK553180/
- https://www.ncbi.nlm.nih.gov/books/NBK470272/
- https://www.ncbi.nlm.nih.gov/books/NBK65779/
- https://www.ncbi.nlm.nih.gov/books/NBK65880/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4239505/
- https://www.health.harvard.edu/diseases-and-conditions/they-found-colon-polyps-now-what
- https://www.nhs.uk/conditions/bowel-polyps/
[/bg_collapse]