Indications of Total Knee Arthroplasty/Total Knee Arthroplasty (TKA) is one of the most cost-effective and consistently successful surgeries performed in orthopedics. Patient-reported outcomes are shown to improve dramatically with respect to pain relief, functional restoration, and improved quality of life. TKA provides reliable outcomes for patients’ suffering from end-stage, tri-compartmental, degenerative osteoarthritis (OA). While OA affects millions of Americans, the knee is the most commonly affected joint plagued by this progressive condition which is hallmarked by a gradual degeneration and loss of articular cartilage. The most common clinical diagnosis associated with TKA is primary OA, but other potential underlying diagnoses include inflammatory arthritis, fracture (post-traumatic OA and/or deformity), dysplasia, and malignancy.[rx][rx][rx]
Types of Total Knee Arthroplasty
There are 2 main types of surgery:
- Total knee replacement – both sides of your knee joint are replaced
- Partial (half) knee replacement – only 1 side of your joint is replaced in a smaller operation with a shorter hospital stay and recovery period.
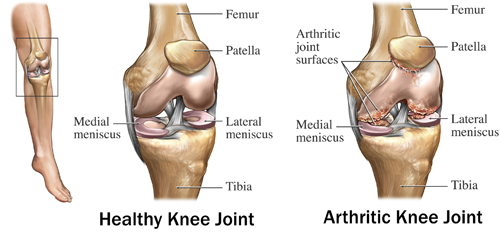
Anatomy and Physiology
The knee is a synovial hinge joint with minimal rotational motion. It is comprised of the distal femur, proximal tibia, and the patella. There are 3 separate articulations and compartments: medial femorotibial, lateral femorotibial, and patellofemoral. The stability of the knee joint is provided by the congruity of the joint as well as by the collateral ligaments. The capsule surrounds the entire joint and extends proximally into the suprapatellar pouch. Articular cartilage covers the femoral condyles, tibial plateaus, trochlear groove, and patellar facets. Menisci are interposed in the medial and lateral compartments between the femur and tibia which act to protect the articular cartilage and support the knee.
The mechanical axis of the femur, defined by a line drawn from the center of the femoral head to the center of the knee, is 3 degrees valgus to the vertical axis. The anatomic axis of the femur, defined by a line bisecting the femoral shaft, is 6 degrees valgus to the mechanical axis of the femur and 9 degrees valgus to the vertical axis.[5] The proximal tibia is oriented to 3 degrees of varus. The varus position of the proximal tibia, along with the offset of the hip center of rotation, results in the weight-bearing surface of the tibia is parallel to the ground. The sagittal alignment of the proximal tibia is sloped posteriorly approximately 5 to 7 degrees. The asymmetry of the natural bony anatomy maintains the alignment of the joint and ligamentous tension. The knee is comprised of 2 separate joints: the tibiofemoral and patellofemoral joints.[rx][rx][rx]
Patellofemoral Joint
The patellofemoral joint (PFJ) functions to increase the lever arm of the extensor mechanism. The patella transmits the tensile forces generated by the quadriceps tendon to the patellar tendon. The maximum contact force between the patella and femoral trochlea occurs at 45 degrees of knee flexion, and joint reaction forces reach 7-times body weight in the position of deep squatting.
The quadriceps muscles provide dynamic stability of the PFJ, and passive anatomic restraints include the following:
-
Medial patellofemoral ligament: Primary passive restraint against lateral translation at 20 degrees of flexion
-
Medial patellomeniscal ligament: Contributes 10% to 15% of the total restraining force
-
Lateral retinaculum: Provides 10% of the total restraining force
Tibiofemoral Articulation
The tibiofemoral articulation transmits body weight from the femur to the tibia and generates joint reaction forces of 3 and 4-times body weight during walking and climbing, respectively. Motion occurs in the sagittal plane from 10 degrees of hyperextension to about 140 to 150 degrees of hyperflexion. Extremes of flexion are often limited secondary to direct contact between the posterior thigh and calf. The tibiofemoral contact point and femoral center of rotation move posteriorly with increasing degrees of flexion in order to optimize knee flexion prior to impingement. Normal gait only requires a range of motion (ROM) from 0 to 75 degrees.
Knee stability in the coronal plane is provided by the lateral collateral ligament (LCL), which resists varus stresses, and the medial collateral ligament, which resists valgus stress forces. In addition, the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) provide resistance to anteriorly directed and posteriorly directed forces at the knee, respectively. Resistance to external rotatory forces is provided by the posterolateral corner structures (PLC).

Indications of Total Knee Arthroplasty
Once considered a procedure reserved for the elderly, low-demand patient population, primary TKA is offered more frequently and provides consistent positive outcomes in younger cohorts of patients. In general, the most common underlying diagnosis associated with performing TKAs across all patient age groups is primary, end-stage, tri-compartmental osteoarthritis.[rx][rx][rx]
TKA is an elective procedure that is, in most cases, reserved for patients experiencing chronic, debilitating symptoms that continue to persist despite the exhaustion of all conservative and nonoperative treatment modalities.
Clinical symptoms of osteoarthritis include
-
Knee pain
-
Pain with activity and improving with rest
-
The pain gradually worsens over time
-
Decreased ambulatory capacity
Clinical evaluation includes
-
Full knee exam including a range of motion and ligamentous testing
-
Knee radiographs include standing anteroposterior, lateral, 45-degree posteroanterior, and skyline view of the patella
Radiographic evidence of osteoarthritis include[rx]
-
Joint space narrowing
-
Subchondral sclerosis
-
Subchondral cysts
-
Osteophyte formation
Conservative treatment includes
-
Non-steroidal anti-inflammatory medication
-
Weight loss
-
Activity modification
-
Bracing
-
Physical therapy
-
Viscosupplementation
-
Intra-articular steroid injection
-
Decreased ambulatory capacity
Clinical evaluation includes
-
Full knee exam including range of motion and ligamentous testing
-
Knee radiographs include standing anteroposterior, lateral, 45-degree posteroanterior, and skyline view of the patella
Radiographic evidence of osteoarthritis include[rx]
-
Joint space narrowing
-
Subchondral sclerosis
-
Subchondral cysts
-
Osteophyte formation
Contraindications of Total Knee Arthroplasty
TKA is contraindicated in the following clinical scenarios
-
Local knee infection or sepsis
-
Remote (extra-articular), active, ongoing infection or bacteremia
-
Severe cases of vascular dysfunction
Absolute
-
Active or latent (less than 1 year) knee sepsis
-
Presence of active infection elsewhere in body
-
Extensor mechanism dysfunction
-
Medically unstable patient
Relative
-
Neuropathic joint
-
Poor overlying skin condition
-
Morbid obesity
-
Noncompliance due to major psychiatric disorder, alcohol, or drug abuse
-
Insufficient bone stock for reconstruction
-
Poor patient motivation or unrealistic expectation
-
Severe peripheral vascular disease
Equipment of Total Knee Arthroplasty
TKA prosthesis designs have been evolving since the 1950s, beginning with Walldius’ design of the first hinged-knee replacement. In the early 1970s, the total condylar prosthesis (TCP) was the first TKA prosthesis designed to resurface all 3 compartments of the knee. The TCP was a posterior-stabilized design. The 4 main categories of TKA prosthesis designs are listed below in the order of increasing levels of constraint by design.[rx][rx][rx]
A TKA system will consist of instrumentation that helps the surgeon prepare the ends of the femur, tibia, and patella to receive an implant. The instrumentation will be specific to the brand and type of implant being used with each company and model having specific intricacies.
In general, the instrumentation will consist of:
-
Intramedullary femoral guide to help establish the distal femoral alignment
-
The distal femoral cutting guide
-
Femoral sizing guide
-
The 4-in-1 femoral cutting guide
-
The extramedullary or intramedullary tibial guide
-
The proximal tibial cutting guide
-
Patella sizing guide
-
Femoral component trial
-
Tibial baseplate trial
-
Patellar button trial
-
Trial plastic bearing
The final implants will come in individual sterile packages and will consist of
-
Femoral component, typically made of cobalt-chrome
-
The tibial component, typically made of cobalt-chrome or titanium
-
Tibial polyethylene bearing, made of an ultra-high molecular weight (UHMW) polyethylene
-
Patellar button, made of UHMW polyethylene
Personnel
-
Anesthesia team
-
Operating room nurse
-
Surgical technician
-
Surgical assistant
Cruciate-Retaining
The cruciate-retaining TKA prosthesis depends on an intact PCL to provide stability inflection. Thus, its use is contraindicated in patients with pre-existing or intra-operatively recognized PCL insufficiency. Caution is given to any patient presenting with at least moderate instability in any plane of motion, especially PLC instability patients. PLC instability predisposes the native PCL in a cruciate-retaining TKA to abnormally high stresses and forces, ultimately leading to early failure and TKA instability requiring revision. Cruciate-retaining TKA is contraindicated in patients suffering from inflammatory arthritic conditions given the increased risk of early PCL attenuation (e.g. Rheumatoid Arthritis).
Proposed advantages of the cruciate-retaining TKA design include:
-
Avoidance of tibial post-cam impingement and dislocation
-
Retaining more normal anatomy theoretically resembles normal knee kinematics
-
Preserved bone stock (less distal femur resected compared to PS TKA prosthesis)
-
Native PCL proprioception
Proposed disadvantages of the cruciate-retaining TKA design include:
-
A tight PCL can lead to early/accelerated polyethylene wear
-
Loose/ruptured PCL results in flexion instability and possible subluxation/dislocation
Multiple meta-analyses have demonstrated satisfactory survivorship and similar outcomes comparing the cruciate-retaining and posterior-stabilized TKA prosthesis designs.
Posterior-Stabilized
The posterior-stabilized TKA design is slightly more constrained and requires the surgeon to sacrifice the PCL. The femoral component contains a cam that is designed to engage the tibial polyethylene post as the knee flexes.
Proposed advantages of the posterior-stabilized TKA design include:
-
Facilitates overall balancing of the knee in the setting of an absent PCL
-
Theoretically, better knee flexion
-
Lower ranges of axial rotation and condylar translation
Proposed disadvantages of the posterior-stabilized TKA design include:
-
Cam jump that can result secondary to a loose flexion gap, or in knee hyperextension
-
Patellar clunk syndrome
-
Tibial post wear and/or fracture
Constrained Nonhinged Design
The constrained nonhinged prosthesis employs a larger tibial post and deeper femoral box, yielding more stability and constraint (within 2 to 3 degrees) in both varus-valgus and internal-external rotatory planes. Indications include collateral ligament attenuation or deficiency, flexion gap laxity, and moderate bone loss in the setting of neuropathic arthropathy. Downsides to this design include not only increased risk of earlier aseptic loosening secondary to the increased inter-component constraint, but also the requirement of more femoral bone resection to accommodate the components.
Constrained Hinged Design
The constrained hinged design is comprised of linked femoral and tibial components. Rotating hinge options allow the tibial bearing to rotate around a yoke that theoretically mitigates the risk of aseptic loosening at the expense of increasing levels of prosthetic constraint. Indications include global ligamentous deficiencies, resections in the setting of tumors, and massive bone loss in the setting of a neuropathic joint.
Other Component Considerations
Modularity and mobile-bearing designs are other noteworthy additional prosthetic design considerations.
Mobile bearing designs allow polyethylene rotation on the tibial baseplate. Although this design concept remains controversial in terms of its generation of reproducibly superior patient-reported outcome measures, advocates cite its utilization and relative indications in younger patient populations secondary to improved wear rates. However, one notable disadvantage includes the potential for bearing spin-out, which is seen especially in the setting of a loose flexion gap.
All-polyethylene tibial base plates contrast the conventional metal tray with polyethylene inserts (i.e. tibial component modularity) that allow surgeons more flexibility for intra-operative adjustments for fine-tuning TKA stability. A surgeon is able to upsize or downsize the polyethylene after the final tibial implant fixation has been achieved between the metal implant and cement (or bone) interfaces. This allows for a final check and balance step which many TKA surgeons appreciate. In contrast, advocates for the all-polyethylene base plates cite significant cost savings and decreased rates of osteolysis when comparing TKA cohorts, especially in the elderly TKA patient populations.[rx][rx]
Preparation
-
Full medical and drug history before surgery
-
Appropriate pre-surgical workup, clearance, and optimization
-
Pre-operative radiographs of the affected knee
-
Pre-operative templating of the affected knee to estimate the component size
-
Primary TKA system of choice
-
Have various final implant sizes ready and available in the hospital
-
Have increasing prosthesis constraint options ready and available in the hospital
-
Have revision total knee replacement system of choice ready and available if needed
-
+/- antibiotic cement, surgeon preference
Nonoperative Treatment Modalities
According to the 2011 American Academy of Orthopaedic Surgeons (AAOS), Evidence-Based Clinical Guidelines for the treatment of symptomatic hip or knee osteoarthritis, strong or moderately strong recommendations for nonoperative treatment modalities include weight loss, physical activity, physical therapy programs, and NSAIDs and/or tramadol. Other modalities that were not supported by moderate or strong evidence but are often considered reasonable alternative treatment options include but are not limited to acupuncture, chondroitin supplementation, hyaluronic acid injections, corticosteroid injections, lateral wedge insoles, and offloading braces.[rx]
Prosthesis design
- tibial component: high-density polyethylene spacer
- femoral component: metallic component, surfaces contoured similarly to the femoral condyles and trochlea
- patellar component: high-density polyethylene; may be metal-backed
Most designs use polymethylmethacrylate (PMMA) cement for fixation. Cementless designs are available, where fixation is achieved initially by friction, then by ingrowth of bone into the prosthesis.
There are many designs in use, but broadly speaking, TKA is characterized by the degree of constraint, polyethylene spacer fixation, and posterior cruciate ligament (PCL) retention or removal.
Degree of constraint
- unconstrained prostheses – most widely used; the patient’s supporting soft tissues help maintain stability
- semi-constrained implants – more stable, decreased range of motion; closely conforming tibial and femoral components
- constrained implants – hinged mechanism; most stable, but most limited range of motion, meaning more mechanical stress and susceptibility to wear, fatigue, and loosening; usually used in:
- revision arthroplasty
- elderly patients with highly unstable ligaments
- combination with tumor resection
Spacer fixation
- fixed bearing: the tibial spacer is fixed in a metal tibial tray
- mobile bearing: a mobile polyethylene insert glides along the surface of the metallic tibial component
PCL retention vs removal
The PCL, an important knee stabilizer, can be:
- retained; this is usually the case with unconstrained prostheses
- removed
- removed and substituted for by a PCL-substituting mechanism in the prosthesis
The decision whether to retain or remove the PCL depends mostly on the surgeon’s preference and experience.
Radiographic features
Plain radiograph
The most cost-effective and commonest method of follow-up. Baseline radiographs should be obtained immediately post-operation.
Normal appearance on routine views:
- AP
- mechanical axis corrected to 0 degrees, results in femoral component placed 5-9 degrees valgus to long axis of femur
- tibial component: aligned perpendicular to long axis of tibia
- polyethylene (radiolucent) spacer in tibiofemoral joint space: equal width medially and laterally; NB: beam angle, patient positioning or post-op flexion contracture may distort this
- lateral
- femoral component: perpendicular to long femoral axis, unless surgeon has chosen to flex component by up to 3 degrees
- tibial component: perpendicular to long tibial axis or posteriorly inclined by up to 5 degrees
- patella: anterior and articular sides parallel to each other. Oblique patella on true lateral view suspicious for subluxation, patella Alta for patellar tendon rupture, and significant patella baja for quadriceps tendon rupture
- skyline Merchant view
- for assessing patellofemoral alignment: patellar component should be centered above femoral component trochlea
CT and MRI
True axial imaging allows assessing for the rotational alignment of the femoral component. To this end, two lines are drawn, which should be parallel:
- transepycondylar line, or axis: drawn between the sulcus of medial epicondyle and peak of the lateral epicondyle
- a second line is drawn across the posterior margins of the femoral component
- if the lines diverge medially, the component is externally rotated: can cause an increased medial flexion gap and result in flexion instability
- if they diverge laterally, the component is internally rotated: early or delayed patellofemoral complications may ensue, especially if internal rotation exceeds 5 degrees
Preoperative Evaluation: Clinical Examination
A thorough history and physical examination are required before performing a TKA in any patient. Patients should be asked about any and all previous interventions and treatments. Prior joint replacements, arthroscopic procedures, or other surgeries around the knee should be considered. Old surgical scars can affect the planned surgical approach. In addition, patients with a history of prior injuries or procedures can present with mechanical axis deformities, retained hardware, or knee instability in any plane. A multitude of factors can impact the TKA prosthesis of choice that is most appropriate for the patient.
We recommend each patient pursuing elective TKA surgery first receive a comprehensive medical evaluation with any appropriate medical optimization tests performed before the TKA procedure. A surgeon must consider the relevant risks and potential benefits of performing TKA on a case-by-case basis.
Physical examination includes evaluation of the overall mechanical axis of the limb. It is critical to ensure hip pathology is either ruled out or at least considered before performing any surgery around the knee. The vascular status of the limb should also be assessed by observing the skin for any chronic venous stasis changes, cellulitis, or even wounds/ulcerations that may be present on the extremity. Distally, the pulses should be symmetric and palpable. Consideration should be given for a vascular surgeon consultation in the preoperative setting in any patient presenting with peripheral vascular disease (PVD). The surgeon should also be aware of the possibility of PVD presenting as knee pain out of proportion in the setting of relatively benign radiographs.
The preoperative range of motion should be noted at the knee and adjacent joints (hip, ankle). The soft tissues should be examined for evidence of gross atrophy, overall symmetry, and ligamentous stability in all planes at the knee joint. It is essential to document the presence of any laxity in the varus/valgus plane and the ability to correct the deformity. These parameters help prepare the surgeon for soft tissue releases that may be required to facilitate mechanical axis correction, as well as plan for additional bone resection that may be needed in the setting of significant contractures.
Preoperative Evaluation: Radiographs
Preoperative radiographs, including a weight-bearing anteroposterior (AP) view, are evaluated for overall mechanical alignment, the presence of deformity, and bone loss. The tibiofemoral angle can help estimate the magnitude of coronal deformity. The femoral resection angle is calculated as the difference between the mechanical and anatomic axis of the femur. The lateral view of the knee is essential for appreciating the native posterior slope of the proximal tibia as well as the presence of posterior osteophytes on the femoral condyles.
The patellofemoral radiographic view is not necessary for TKA templating but allows the surgeon to evaluate the magnitude of patellofemoral arthritis and deformity. In cases of advanced patellofemoral deformity, osteophyte removal may be needed prior to attempting to evert the patella during the procedure. In addition, a surgeon can plan for a possible lateral release to improve patellar tracking.
Technique
The goal of TKA is the same regardless of surgeon, implant, or technique. The variability in the procedure lies in the technique. Some of the variations in the operative technique for TKA are listed below.
-
General anesthesia versus regional anesthesia
-
Tourniquet versus tourniquet-less surgery
-
Standard versus patient-specific instrumentation
-
Standard versus patient-specific implants
-
Traditional versus robotic-assisted TKA
-
Traditional versus navigation-assisted TKA
-
Traditional versus sensor-assisted TKA
-
Measured resection versus gap balancing
-
Cruciate-retaining implant versus cruciate stabilized the implant
-
Resurfaced versus non-resurfaced patella
-
Cement versus cement-less (press fit) TKA
Surgical Approaches
The most common approaches for the standard primary TKA procedure include the medial parapatellar, midvastus, and subcastes approach. The medial parapatellar approach is commonly utilized and entails proximal dissection through a medial cuff of the quadriceps tendon to facilitate superior tissue quality closure at the conclusion of the procedure. Distally, a meticulous, continuous medial subperiosteal dissection sleeve is performed while maintaining intimacy with the proximal tibial bone. The extent of dissection is often dictated by the anticipated amount of deformity to be corrected. In general, this medial release is aggressive in cases of severe varus deformity, and most minimal in cases of moderate to advanced valgus knee deformity. The medial meniscus is also resected with this sleeve of soft tissue.[rx][rx][rx]
Alternatives to the standard medial parapatellar arthrotomy include the midvastus and subvastus approaches. The midvastus approach spares the quadriceps tendon. Instead, the vastus medialis obliquus (VMO) muscle belly is dissected along a trajectory directed toward the superomedial aspect of the proximal pole of the patella.
The subvastus approach also spares the quadriceps tendon and lifts the muscle belly of the VMO off the intermuscular septum. The subvastus approach preserves the vascularity of the patella and is cautioned as it can limit exposure in particularly challenging cases or in particularly obese patients.
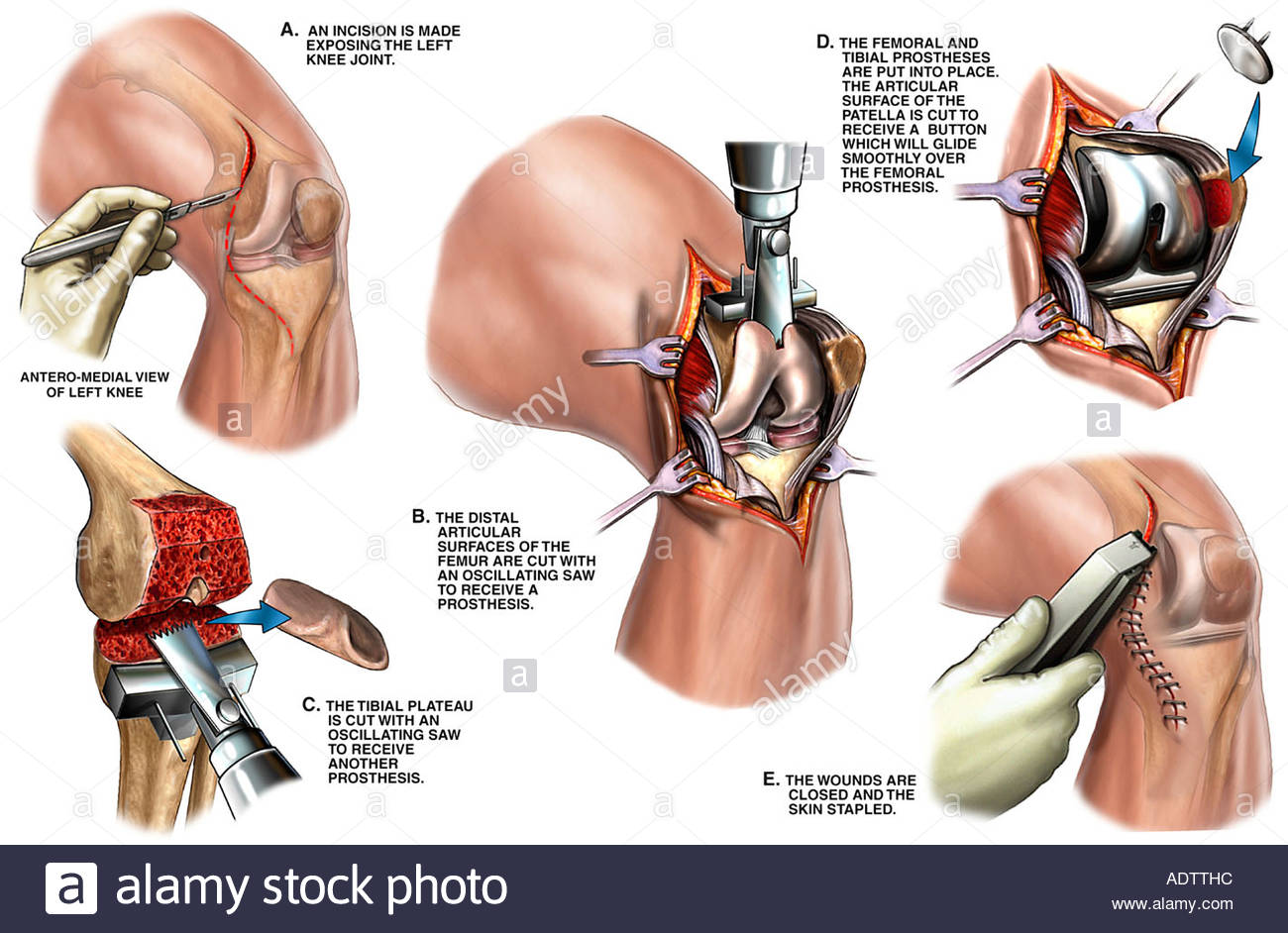
Procedural Steps
Depending on surgeon preference, the specific order of bone resections and soft tissue releases will vary. However, a general overview of a preferred method is the goal of this technical summary of the TKA procedure.
Once the arthrotomy is complete, the patella is everted, and the knee is flexed with additional soft tissue releases required prior to achieving knee dislocation. If the surgeon elects to proceed with the femur first, an intramedullary (IM) drill is utilized in order to gain access to the femoral canal for the utilization of a distal femoral IM jig. The angle set on the guide is based on the patient-specific preoperative evaluation (AP Xray), generally yielding 5 or 7 degrees of valgus. Although system-specific, most surgeons prefer resecting 9 to 10 mm of the distal femur.
Next, the proximal tibia is cut utilizing an IM or extramedullary (EM) guide with the goal of cutting the bone perpendicular (or within 2 to 3 degrees of varus for surgeons aiming for an “anatomic” TKA procedure) to the tibial axis. We prefer an IM guide and a perpendicular tibial cut. The rotation is set referencing the medial one-third of the tibial tubercle (proximally) and a point slightly medial to the center of the ankle joint (distally). This alignment is also referenced with the second ray of the foot and the tibial crest.
Once the tibial cut is performed, the extension gap can be assessed. A spacer block is then inserted with the knee in full extension, and the overall balance of the knee is assessed using an alignment rod to facilitate and verify overall varus-valgus and tibial slope parameters achieved.
Next, the flexion gap is attained after utilizing an AP sizing guide that is positioned with respect to the bony landmarks on the femur (usually Whiteside’s line or the native transepicondylar axis [TEA]). Depending on the anterior or posterior referencing style of the operating surgeon, the flexion gap is set and adjusted as needed utilizing the system-specific incremental sizing adjustments available with respect to the cutting guides. Prior to making the bony cuts, the flexion gap should be visualized, and soft tissue balancing appreciated. A spacer block can facilitate this assessment. The surgeon should ensure a rectangular flexion gap will be the ultimate result after the bone resections. After satisfactory check and balancing steps are verified, the anterior, posterior, anterior chamfer and posterior chamfer cuts are made. Care is taken to protect the collateral soft tissue structures (LCL, MCL) with retractors.
Next, the intercondylar notch cut is made perpendicular to the TEA. The attention is again turned back to the proximal tibia to finish preparation, sizing, and rotational alignment. One must be cautious to avoid internal rotation and/or component overhang which can lead to inferior TKA results. The femoral and tibial trial implants are impacted, and a provisional spacer trial is inserted. The knee is reduced and assessed for stability from 0 degrees of extension through mid-flexion stability.
If planning to resurface the patella, the resection is recommended after first appreciating the native anatomy and size of the entire patellofemoral joint. Inferior TKA outcomes can result from either over-resection, which can compromise implant-bone stock and lead to patella fracture, or under-resection, which can lead to chronic postoperative pain secondary to an overstuffed PFJ.
Finally, the stability parameters are again verified, and patellar tracking is appreciated and must pass intraoperative tracking tests. Most surgeons either use a natural range of motion tracking test to ensure the TKA passes the “no thumb” test, or a towel clip technique can be used.
Patellar maltracking, most commonly occurring laterally, can most often be corrected with a standard lateral release. In more severe cases or in scenarios consistent with component malalignment, consideration should be given to the correction of component position(s).
Wound Closure
The most recent literature remains controversial with respect to the ideal position of the knee and suture material utilized during the TKA closure. Attention to detail is required and a methodical closure is unanimously advocated. A preferred method includes closure with uni- or bi-directional barbed suture for the arthrotomy, deep fascial, and deep dermal/subcutaneous layers. Staples or monocryl can be used for the skin. A sterile dressing is then applied and left in place without being changed for the first 7 days. In addition, a minimal website/ace soft wrap dressing is applied to the knee for, at most, 24 hours to facilitate the appropriate balance between wound healing and postoperative movement of the knee.
Other Considerations
Topical tranexamic acid (TXA) is the preferred application while waiting for the cement to fully harden and prior to dropping the tourniquet. In addition, other controversial technical modalities in TKA include the use of a tourniquet, cementing the patella, femoral, and/or tibial components, as well as incorporating a betadine soak to the wound as part of the copious saline irrigation that is applied prior to closure of the arthrotomy and surgical wound. Preferred techniques include the use of a tourniquet, cementing all components, and saline-only copious pulsatile irrigation prior to arthrotomy closure.
Post-operative Rehabilitation
The length of postoperative hospitalization is 5 days on average depending on the health status of the patient and the amount of support available outside the hospital setting.[rx] Protected weight bearing on crutches or a walker is required until specified by the surgeon[rx] because of weakness in the quadriceps muscle[rx] In the immediate post-operative period, up to 39% of knee replacement patients experience inadequate pain control.[rx]
To increase the likelihood of a good outcome after surgery, multiple weeks of physical therapy is necessary. In these weeks, the therapist will help the patient return to normal activities, as well as prevent blood clots, improve circulation, increase range of motion, and eventually strengthen the surrounding muscles through specific exercises. Whether techniques such as neuromuscular electrical stimulation are effective at promoting gains in knee muscle strength after surgery are unclear.[rx] Often a range of motion (to the limits of the prosthesis) is recovered over the first two weeks (the earlier the better). Over time, patients are able to increase the amount of weight-bearing on the operated leg, and eventually are able to tolerate full weight-bearing with the guidance of the physical therapist.[rx] After about ten months, the patient should be able to return to normal daily activities, although the operated leg may be significantly weaker than the non-operated leg.[rx]
For post-operative knee replacement patients, immobility is a factor precipitated by pain and other complications. Mobility is known as an important aspect of human biology that has many beneficial effects on the body system.[rx] It is well documented in the literature that physical immobility affects every body system and contributes to functional complications of prolonged illness.[rx] In most medical-surgical hospital units that perform knee replacements, ambulation is a key aspect of nursing care that is promoted to patients. Early ambulation can decrease the risk of complications associated with immobilization such as pressure ulcers, deep vein thrombosis (DVT), impaired pulmonary function, and loss of functional mobility.[rx] Nurses’ promotion and execution of early ambulation on patients has found that it greatly reduces the complications listed above, as well as decreases length of stay and costs associated with further hospitalization.[rx] Nurses may also work with teams such as physical therapy and occupational therapy to accomplish ambulation goals and reduce complications.[rx]
Continuous passive motion (CPM) is a postoperative therapy approach that uses a machine to move the knee continuously through a specific range of motion, with the goal of preventing joint stiffness and improving recovery.[rx][rx] There is no evidence that CPM therapy leads to a clinically significant improvement in range of motion, pain, knee function, or quality of life.[rx] CPM is inexpensive, convenient, and assists patients in therapeutic compliance. However, CPM should be used in conjunction with traditional physical therapy.[rx] In unusual cases where the person has a problem that prevents standard mobilization treatment, then CPM may be useful.[rx]
Cryotherapy, also known as ‘cold therapy’ is sometimes recommended after surgery for pain relief and to limit swelling of the knee. Cryotherapy involves the application of ice bags or cooled water to the skin of the knee joint. However, the evidence that cryotherapy reduces pain and swelling is very weak and the benefits after total knee replacement surgery have been shown to be very small.[rx]
Some physicians and patients may consider having ultrasonography for deep venous thrombosis after knee replacement.[rx] However, this kind of screening should be done only when indicated because to perform it routinely would be unnecessary health care.[rx] If a medical condition exists that could cause deep vein thrombosis, a physician can choose to treat patients with cryotherapy and intermittent pneumatic compression as a preventive measure.
Neither gabapentin nor pregabalin has been found to be useful for pain following a knee replacement.[rx] A Cochrane review concluded that early multidisciplinary rehabilitation programs may produce better results at the rate of activity and participation.[rx]
Complications
TKA complications result in inferior outcomes and patient-reported satisfaction scores. Although TKA remains a reliable and reproducibly successful surgery in patients suffering from debilitating advanced degenerative arthritic knees, reports still cite that up to 1 in 5 patients who have undergone primary TKA remain dissatisfied with the outcome.[rx][rx][rx]
Periprosthetic Fracture
TKA periprosthetic fractures (PPFs) are further characterized by location and residual stability of the implants. Distal femur PPFs occur at a 1% to 2% rate, and risk factors include compromised patient bone quality, increased constrained TKA components, and while controversial, anterior femoral notching is a potential risk factor for postoperative fracture.
Tibial PPFs occur at a 0.5% to 1% rate, and risk factors include a prior tibial tubercle osteotomy, component malposition and/or loosening, as well as utilization of long-stemmed components. Patellar PPFs occur less frequently in unresurfaced TKA cases, and incidence rates range from 0.2% up rates as high as 15% or 20%. Risk factors for fracture include osteonecrosis, technical errors in asymmetric or over-resection, and implant-related associations including the following:
-
Central, single peg implants
-
Uncemented fixation
-
Metal-backed components
Aseptic Loosening
TKA aseptic loosening occurs secondary to a macrophage-induced inflammatory response resulting in eventual bone loss and TKA component loosening. Patients often present with pain that is increased during weight-bearing activity and/or recurrent effusions. Patients may have minimal pain at rest or with range of motion. Serial imaging and infectious labs are required to appropriately work up these conditions which eventually are treated with revision surgery if symptoms persist and the patient is considered a reasonable surgical candidate. The steps in aseptic loosening include: particulate debris formation, macrophage-induced osteolysis, micromotion of the components, and dissemination of particulate debris.
Wound Complications
The TKA postoperative wound complication spectrum ranges from superficial surgical infections (SSIs) such as cellulitis, superficial dehiscence and/or delayed wound healing to deep infections resulting in full-thickness necrosis resulting in returns to the operating room for irrigation, debridement (incision and drainage), and rotational flap coverage.
Periprosthetic Joint Infection
The incidence of prosthetic total knee infection (TKA PJI) following primary TKA is approximately 1% to 2% as reported in the literature. Risk factors include patient-specific lifestyle factors (morbid obesity, smoking, intravenous [IV] drug use and abuse, alcohol abuse, and poor oral hygiene) and patients with a past medical history consisting of uncontrolled diabetes, chronic renal and/or liver disease, malnutrition, and HIV (CD4 counts less than 400). PJI is the most common reason for revision surgery.
The most common offending bacterial organisms in the acute setting include Staphylococcus aureus, Staphylococcus epidermidis, and in chronic TKA PJI cases, coagulase-negative staphylococcus bacteria. Treatment in the acute setting (less than 3 weeks after index surgery) can be limited to incision and drainage, polyethylene exchange, and retention of components. In addition, IV antibiotics are utilized for up to 4 to 6 weeks duration. Outcomes vary and are often influenced by multiple intraoperative, patient-related factors, and offending bacterial organism, but studies site a 55% successful outcome rate.
More aggressive treatments, especially in the setting of presentation beyond the acute (3 to 4-week time point) include a 1 or 2-stage revision TKA procedure with interval antibiotic spacer placement. The surgeon must ensure and document evidence of infection eradication.
Other Complications and Considerations
Other potential complications after TKA are beyond the scope of this review but include:
-
TKA instability – can occur in the coronal or sagittal plane(s). Also, consideration is given for patellar maltracking or other PFJ issues (for example, overstuffing the joint) in the postoperative setting when patients complain of persistent anterior knee pain
-
Extensor mechanism disruption or rupture
-
Patellar clunk syndrome – Often occurs 12 months after TKA and is associated with popping, catching during knee extension. It is caused by nodule formation on the posterior quad tendon near its insertion on the patella. Patellar clunk syndrome is associated with posterior stabilized knee design. The cause of scar tissue formation is unknown but the pain results from tissue entrapment in the intercondylar notch. Treatment is surgical, either arthroscopic or open debridement/synovectomy. Conservative measures are often unsuccessful. physical therapy may help with quad strengthening after surgery but is not curative. Recurrence after surgical treatment is rare. More aggressive intervention such as revision TKA is often not warranted in the absence of component malposition.
- Peroneal nerve palsy – One of the most common complications after TKA to correct the valgus deformity. During soft tissue balancing of a valgus knee, the iliotibial band preferentially affects the extension space more than flexion space and inserts on Gerdy’s tubercle. The popliteus is preferentially affected flexion space more than extension space.
-
Stiffness
-
Vascular injury and bleeding
-
Metal hypersensitivity
- Infection, superficial and deep
-
Blood clot
-
Pulmonary embolism
-
Fracture
-
Dislocation
-
Instability
-
Osteolysis resulting in component loosening
-
Pain
-
Stiffness
-
Vascular injury
-
Nerve injury
Commonly Required and Suggested Home Preparations
Deep bending and squatting can lead to knee injuries during the recovery period. A patient can minimize these risks by making advanced arrangements and preparing his or her home. For example:
- Arrange for a spouse, friend or other caregiver to provide meals and help around the house.
- Arrange for transportation, as most patients cannot drive for the first 4 to 6 weeks after surgery.
- Stock up on pre-made meals and toiletry items to avoid having to run errands post-surgery.
- If possible, arrange to spend sleeping and waking hours on the same floor in order to avoid stairs.
- If possible, adjust the bed height (not too high or too low) to help ease the transition in and out of bed.
- Take away or move anything that might be tripped over, such as area rugs or electrical cords.
- Make sure all stairs have sturdy railings.
- Install small rails or grab bars near toilets and in showers.
- Install a modified toilet seat; a higher seat will put less stress on the knees and make it easier to sit down and get up.
- Put a small stool in shower to avoid standing on a slippery surface.
- Have a comfortable, supportive chair with an ottoman to keep leg elevated for intervals.
- Have cold packs on hand to help alleviate swelling.
- Consider practicing using walkers, canes and other assistive devices ahead of time to ensure proficiency using them.
References
[bg_collapse view=”button-orange” color=”#4a4949″ expand_text=”Show More” collapse_text=”Show Less” ]
- https://www.ncbi.nlm.nih.gov/books/NBK499896/
- https://www.ncbi.nlm.nih.gov/books/NBK507914/
- https://www.ncbi.nlm.nih.gov/books/NBK538208/
- https://www.ncbi.nlm.nih.gov/books/NBK11960/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5790068/
- https://www.ncbi.nlm.nih.gov/books/NBK507864/
- https://www.ncbi.nlm.nih.gov/books/NBK507864/
- https://www.ncbi.nlm.nih.gov/books/NBK507864/
- https://www.nhs.uk/conditions/knee-replacement/
[/bg_collapse]