What Is Osteophyte?/Osteophyte formation is in addition to joint space narrowing, subchondral sclerosis and subchondral cyst formation one of the main radiographic features of OA and an important criterium for this disease. Osteophytes can form early in the development of OA and can be seen prior to joint space narrowing.
An osteophytes is “a fibrocartilage-capped bony outgrowth”. Osteophytes are exostoses (bony projections) that form along joint margins. They should not be confused with enthesophytes, which are bony projections that form at the attachment of a tendon or ligament.[rx]Three types of osteophytes are known, the traction spur at the insertion of tendons and ligaments, the inflammatory spur, represented by the syndesmophyte at the insertion of ligaments and tendons to the bone as can be seen in ankylosing spondylitis; and the genuine osteophyte or osteochondrophyte (chondro-osteophyte) arising in the periosteum overlying the bone at the junction between cartilage and bone[rx].
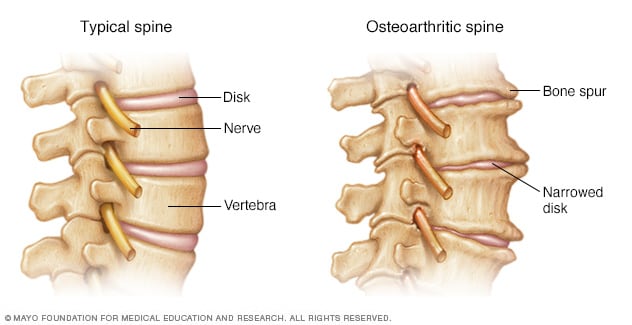
Osteophytes are commonly referred to as bone spurs that form along the joint margin. In the spine, osteophytes are universally considered to be the principal agents that compress the spinal cord or roots and result in symptoms of radiculopathy and of myelopathy. The primary aim during surgery for degenerative spine has been either removal of osteophyte for direct decompression of the neural structures or indirectly to perform surgical procedures that will increase the spinal canal dimension and reduce the pinching effect of the osteophyte.
Types of Osteophytes
Both osteophytes and enthesophytes are considered to be a bone’s reaction to stress:
- Marginal osteophyte – endochondral ossification due to vascularization of subchondral bone marrow. An outgrowth of at the margin of the joints producing lip of bone.
- Periosteal ( synovial) osteophyte – Intramembranous types of ossification due to stimulation of periosteal membrane with appositional bone formation. Thickening of intraarticular cortices producing buttressing.
- Central osteophyte – Endochondral ossification due to vascularization of the subchondral bone marrow. The outgrowth of the central area of the joints producing bumpy contour.
- Capsular osteophyte – Capsular traction lips of bone extending along the direction of capsular pull.
- Spinal Osteophytes – are typically the result of excess friction. In the spine, osteophytes are often found where vertebral bones meet to form a joint (facet joints).
- Enthesophytes – are bone spurs that develop where ligaments and tendons attach to bone (a point called the enthesis). Located at an attachment of a ligament or tendon, not associated with a joint. A chronic strain, injury, or disease causes a ligament or tendon to become damaged and inflamed. If inflammation occurs at the attachment point, a bone spur may develop.
- Syndesmophyte – paravertebral ossifications that run parallel with the spine cf. osteophytes which typically protrude perpendicular to the spine.
Bone spurs can affect your
- Knee (making it hard to straighten your leg).
- Spine (pressing against your spinal cord and causing weakness or loss of feeling in your arms and legs).
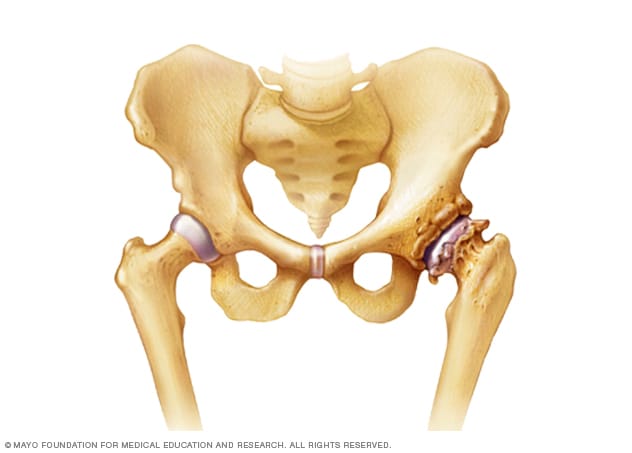
- Hip (making it hard to move your hip).
- Shoulder (causing damage to your rotator cuff, a group of muscles and tendons that enable your shoulder to move).
- Fingers.
- Heel or foot.
A range of bone-formation processes is associated with aging, degeneration, mechanical instability, and disease (such as diffuse idiopathic skeletal hyperostosis).
Causes of Osteophytes
Bone spurs typically cause back pain one of three ways:
- Joint inflammation. Bone spurs of the joints of the spine (facet joints) can cause adjacent vertebrae to grind against each other, resulting in friction and inflammation. The inflammation can lead to pain, stiffness, and other symptoms.
- Compression of a nerve root. The development of bone spurs can cause narrowing of the neural foramina, where the nerve roots exit the spinal column. With less space, the nerve roots may become compressed. Nerve root compression can cause paresthesia (tingling) if they become compressed. If the nerve root becomes inflamed, pain may occur.
- Compression of the spinal cord. Bone spurs can grow into the spinal canal, where the spinal cord travels, leaving less space for the spinal cord. Compression of the spinal cord can cause weakness, strength loss, pain and other symptoms.
- Osteophyte formation has been classically related to any sequential and consequential changes in bone formation that is due to aging, degeneration, mechanical instability, and disease (such as diffuse idiopathic skeletal hyperostosis). Often osteophytes form in osteoarthritic joints as a result of damage and wear from inflammation. Calcification and new bone formation can also occur in response to mechanical damage in joints.[rx]
- Osteophytes tend to form when the joints have been affected by arthritis.
- Osteoarthritis damages cartilage, the tough, white, flexible tissue that lines the bones and allows the joints to move easily.
- Osteoarthritis is most common in the knees, hips, spine and small joints of the hands and base of the big toe.
- As the joints become increasingly damaged, new bone may form around the joints. These bony growths are called osteophytes.
- Osteophytes can also form in the spine as a result of ankylosing spondylitis, a type of arthritis that specifically affects the spine.
- Increased age
- Disc degeneration
- Joint degeneration
- Sports injury or another joint injury
- Poor posture
- Genetics
- Congenital skeletal abnormalities
How Does a Degenerated Disc Lead to Bone Spurs?
A degenerated disc is likely to lead to instability in the spine, and instability is likely to lead to the type of bone spurs called enthesophytes.
- An enthesis is a piece of connective tissue that attaches another soft tissue, such as a ligament, to a bone.
- As intervertebral disc material slowly wears out, nearby ligaments holding vertebra together loosen. The spine loses some stability.
- Instability puts extra stress on the ligaments, causing them to become inflamed. They may also naturally thicken to decrease excess motion and regain some stability.
- Inflammation occurs at the enthesis.
- The inflammation at the enthesis affects the vertebra’s bone growth. Vertebral bone cells are deposited where they would not be normally, causing the enthesis tissue to calcify.
- This calcification forms a bone spur.
Symptoms of Osteophytes
Most bone spurs cause no signs or symptoms. You might not realize you have bone spurs until an X-ray for another condition reveals the growths. In some cases, though, bone spurs can cause pain and loss of motion in your joints.
Symptoms vary depending on where the spur is located:
- Pain in the affected joint
- Pain or stiffness when you try to bend or move the affected joint
- Weakness, numbness, or tingling in your arms or legs if the bone spur presses on nerves in your spine
- Muscle spasms, cramps, or weakness
- Bumps under your skin, seen mainly in the hands and fingers
- Trouble controlling your bladder or bowels if the bone spur presses on certain nerves in your spine (a symptom that’s seen very rarely)
- Heel pain when standing, walking, jogging, or running. Some people describe the pain as feeling like pins sticking into the bottom of their feet.
- Knee pain when extending or bend the leg.
- Hip pain when moving the hip, and a reduction in the hip’s range of motion.
- Spine weakness or numbness in the arms or legs caused by the bone spur pinching the spinal cord or its nerve roots.
- Shoulder limited movement of the shoulder; swelling or tears in the rotator cuff.
- Finger pain when moving the finger; the finger joint may look enlarged and knobby.
Specific symptoms depend on where the bone spurs are. Examples include
- Knee – Bone spurs in your knee can make it painful to extend and bend your leg.
- Spine- On your vertebrae, bone spurs can narrow the space that contains your spinal cord. These bone spurs can pinch the spinal cord or its nerve roots and can cause weakness or numbness in your arms or legs.
- Hip – Bone spurs can make it painful to move your hip, although you might feel the pain in your knee. Depending on their placement, bone spurs can reduce the range of motion in your hip joint.
- rub against other bone or tissue
- restrict movement
- squeeze nearby nerves
- the spine can cause pain and stiffness in the bac
- the neck can pinch a nearby nerve and cause pain, pins and needles, numbness or weakness in the arms
- the shoulder can limit the space available for tendons and ligaments and may be linked to tendonitis or a rotator cuff tear
- hip and knee can reduce the range of movement and are often associated with painful arthritis
- the knee may cause pain when you bend and extend your leg
- fingers can cause lumps
Bone Spurs in the Neck (Cervical Spine)
Depending on the location of bone spurs in the neck, people may notice:
- Dull, achy pain in the neck that gets better with rest
- Radiating pain into one or both shoulders
- Pain, numbness, or tingling in one or both arms
- Weakness in the upper limbs
- Headaches that originate with a dull ache at the back or one side of the neck and travel up the back of the head
- Numbness, tingling, and weakness in both shoulders, arms, and/or hands may be signs of spinal stenosis, commonly caused by bone spurs.
- Develop slowly over time
- Are made worse with activity
- Improve with rest
Bone Spurs in the Low Back (Lumbar Spine)
When bone spurs cause spinal stenosis in the lower spine, people may report feeling:
- Dull pain in lower back when standing or walking
- Pain, numbness, or tingling into the buttocks and back of the thigh(s)
- Weakness in one or both legs
- Pain relief when bending forward and flexing at the waist, such as leaning over a shopping cart or over a cane
Diagnosis of Osteophytes
Standards for osteophyte scoring
| Score | Description |
|---|---|
| Vertebral body | |
| Stage 0 | No evidence of osteoporosis; smooth rim with no scalloping or osteophytes points (no reactive bone activity) |
| Stage 1 | Minor evidence of osteoporosis; one or two small osteophyte points (< 2 mm in length and width) but no larger osteophytes that protrude above the rim and/or the beginnings of arthritic lipping but no horizontally-projecting lipping |
| Stage 2 | More developed osteoporosis; three or more small osteophyte points or larger osteophytes and/or horizontally-projecting arthritic lipping at least 3 mm in length or the fusion of multiple osteophytes points that protrude |
| Stage 3 | Arthritic lipping/fused osteophytes that extend out either superiorly or inferiorly at least 3 mm in height (towards the center of the vertebral body or the adjacent vertebra) |
| Stage 4 | Either partial or complete fusion of arthritic lipping/fused osteophytes between adjacent vertebrae |
| Lamina | |
| Stage 0 | No evidence of osteoporosis; rolling/smooth contour allowable along the laminar margin but no pronounced bumps, osteophytes points, or raised ridge |
| Stage 1 | Minor evidence of osteoporosis; one or two small osteophyte points (< 2 mm in length and width) but no larger osteophytes |
| Stage 2 | More developed osteoporosis; three or more small osteophyte points or one or two larger osteophytes |
| Stage 3 | Three or larger osteophytes and/or fused osteophytes (multiple points coming off 1 or more osteophytes) that cover < 50% of the area created by the articular facet and the midline |
| Stage 4 | Three or more larger osteophytes and/or fused osteophytes that cover 50% or more of the area created by the articular facet and the midline |
Frequency and False-Positive Rates of Marginal Osteophytes in Detecting Cartilage Lesions Within the Same Compartment of the Knee Joint
| Grade of Osteophyte and Compartment |
Frequency of Osteophytes (%) | No. of Positive Findings/Total Findings | False-Positive Rate (%) |
|---|---|---|---|
| Grade 1 | |||
| Patellofemoral | 30.6 | 132/153 | 13.5 |
| Medial | 25.4 | 88/127 | 17.3 |
| Lateral | 19.6 | 60/98 | 14.3 |
| Grade 2 | |||
| Patellofemoral | 6.8 | 33/34 | 0.7 |
| Medial | 9.6 | 47/48 | 0.5 |
| Lateral | 9.4 | 40/47 | 3.0 |
| Grade 3 | |||
| Patellofemoral | 5.6 | 27/28 | 0.7 |
| Medial | 5.4 | 26/27 | 0.5 |
| Lateral | 7.4 | 32/37 | 2.2 |
| All grades | |||
| Patellofemoral | 43.0 | 192/215 | 14.6 |
| Medial | 40.4 | 161/202 | 18.1 |
| Lateral | 36.4 | 132/182 | 21.2 |
Note—False-positive osteophytes were defined as osteophytes present in compartments with normal cartilage.
Imaging
Diagnostic medical imaging may also be ordered:
- X-rays – of the spine can show bone spur formation and signs of spinal degeneration. X-rays can also help the physician determine if additional medical imaging, such as a CT or MRI scan, is needed.
- A computerized tomography scan (CT scan) – is the preferred test to accurately assess bony anatomy, especially in a spine that has had prior surgery. A CT scan provides multiple cross-sectional x-rays of the body. When used with contrast injected into the fluid that normally bathes the spine, the cerebrospinal fluid (located in the intrathecal space), CT scans better demonstrate nerves and soft tissue in addition to bone. A CT scan with contrast is called a CT myelogram.
- MRI scan is the preferred test to observe soft tissues such as discs, nerve roots, ligaments, muscles, tendons and cartilage. Unlike x-rays and CT scans, MRIs do not involve radiation. MRIs take more time and tend to be more expensive than x-rays and CT scans.
- Electroconductive tests. These tests measure how fast your nerves send electrical signals. They can show the damage bone spurs have caused to nerves in your spinal canal.
Treatment / Management of Osteophytes
Non-pharmacologic treatments include specific exercises, physical therapy, bracing, acupuncture, and weight reduction.
- Short periods of rest – Activity may flare up inflammation in the joints. Short periods of rest can give the inflammation time to recede.
- Physical therapy and exercise – Physical therapy, exercise, and manipulation (performed by chiropractors [DC], osteopaths [DO], and physical therapists [PT]), may alleviate back pain associated with bone spurs. These rehabilitation therapies attempt to restore flexibility and strength to the spine, improve posture and decrease nerve root compression.
- Spinal manipulation – If the pain and inflammation caused by bone spurs are related to abnormal alignment and movement patterns in the spine, a spinal adjustment may help relieve symptoms. Chiropractors, osteopaths, and physical therapists use their hands or small instruments to apply pressure over the skin of vertebrae and manipulate the spine. The goal is to increase range of motion, reduce nerve irritability, and improve function. Spinal manipulation is not appropriate for everyone. A careful medical history, physical examination, and discussion of the risks and benefits of manipulation should occur prior to this type of treatment.
- Weight loss – Losing excess weight can take the pressure off the spine, reducing friction between the vertebrae’s facet joints and decreasing the likelihood of pain. Achieving an appropriate weight is especially effective in taking pressure off the lower back.
- Physical therapy – A physiotherapist may also be able to help you by recommending exercises that can strengthen the muscles surrounding the problem area, and by helping to improve your range of movement.
Medication
- NSAIDs (nonsteroidal anti-inflammatory drugs) – If you’re in pain, painkillers you can buy from a pharmacy or shop, such as paracetamol or ibuprofen, may help. Ibuprofen is a non-steroidal anti-inflammatory drug (NSAID), which can also help reduce any swelling and inflammation. Frequently used medications include oral and topical non-steroidal anti-inflammatory drugs (NSAIDs), topical capsaicin, and duloxetine. Corticosteroids can be injected directly into the joint.
- Duloxetine – can be useful for patients that have medical contraindications to NSAID use. If both non-pharmacological and pharmacological management fails, intra-articular corticosteroid injections might provide symptom relief. Opioids should be avoided. [rx]
- Steroid Injections – Fluoroscopically guided, contrast-enhanced spinal injection procedures that target the presumptive source of spinal pain can help decrease pain and inflammation. In addition, depending on whether local anesthetic is used as part of the injection into the spine, the procedure can help an astute clinician identify or narrow down the source of a patient’s pain.
- A spinal injection – may not completely relieve a patient’s pain but may provide enough relief to allow the progression of rehabilitation. Patients should avoid receiving more than 3 injections into any one joint over a short period of time. In addition, if the first injection provides no relief, there is no evidence that further injections into the same structure will provide a better result.
- Muscle relaxant
- Physical therapy; combining passive and active modalities
- Chiropractic
- Acupuncture
If these nonsurgical treatments fail to treat pain due to bone spurs, a patient may be referred to a spinal surgeon.
Spine Surgery for Bone Spurs
In the spine, removal of an osteophyte may be necessary for direct decompression of nerve impingement or to increase spinal canal width to reduce pinching by the osteophyte.
Spine surgery may be recommended if the nerve or spinal cord compression is causing unremitting pain and/or loss of motor/sensory function. Surgery for bone spurs involves removing tissue to relieve pressure on the spinal cord and/or nerve roots. For example:
- Bone spur removal – During this surgery special tools are used to remove bone spurs from the vertebra(e). Since it is possible for the bone spurs to grow back, and because there may be more than just bone spurs contributing to symptoms, a surgeon may suggest another surgical procedure, such as a laminectomy or foraminotomy.
- Laminectomy – A laminectomy is designed to relieve pressure on the spinal cord caused by central spinal stenosis. During surgery, a portion of the affected vertebra called the lamina and spinous process at the back of the spine is removed. With this small piece of the spinal canal wall removed, there is more room for the spinal cord.
- Foraminotomy – A foraminotomy is designed to relieve pressure on a nerve root. Every nerve root passes through an intervertebral foramen, a bony, hollow archway between 2 adjacent vertebrae. During a foraminotomy, bone tissue around the foramen is cut away or shaved down, enlarging the foramen space. This procedure creates more space for the nerve root, relieving nerve root compression.
Tips for pain management
Take the following steps to help control your bone spur pain:
- Lose weight, if you’re overweight or obese, to relieve the burden on your joints.
- Wear shoes that offer good foot support to cushion your feet and other joints when you walk.
- Start physical therapy to learn exercises that will strengthen the muscles around the joint and stabilize it, too.
- Maintain proper posture when standing or sitting to help preserve back strength and keep your spine properly aligned.
- Use over-the-counter painkillers, such as ibuprofen, when inflammation and pain flare up because of a bone spur. Ask your doctor before taking an anti-inflammatory drug.
- Wear shoes with a wide toe box, good arch support, and enough cushion to pad each step. Get your shoes fitted by a professional so they don’t rub against your feet when you walk. Wear thick socks to prevent your shoes from rubbing.
- Eat a well-rounded diet with plenty of calcium and vitamin D to protect your bones.
- Do regular weight-bearing exercises like walking or stair-climbing to keep your bones strong.
- Try to keep the extra pounds off.
References
[bg_collapse view=”button-orange” color=”#4a4949″ expand_text=”Show More” collapse_text=”Show Less” ]
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3248663/
- https://www.ncbi.nlm.nih.gov/books/NBK518992/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3606549/
- https://www.ncbi.nlm.nih.gov/books/NBK541049/
- https://www.ncbi.nlm.nih.gov/books/NBK538204/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1819511/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3872653/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3868137/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6334768/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6624344/
- https://www.sciencedirect.com/science/article/pii/S106345840600327X
- https://www.verywellhealth.com/what-are-osteophytes-bone-spurs-189347
- https://www.mayoclinic.org/diseases-conditions/bone-spurs/diagnosis-treatment/drc-20370216
- https://www.nhs.uk/conditions/osteophyte/
- https://www.medicinenet.com/bone_spurs/article.htm
- https://www.verywellhealth.com/what-are-osteophytes-bone-spurs-189347
- https://www.mayoclinic.org/diseases-conditions/bone-spurs/diagnosis-treatment/drc-20370216
- https://www.sciencedirect.com/topics/medicine-and-dentistry/osteophyte
- https://www.upmc.com/services/orthopaedics/conditions-treatments/bone-spurs
- https://www.webmd.com/pain-management/what-are-bone-spurs
- https://www.cooperhealth.org/services/bone-spurs-osteophytes
- https://www.arthritis-health.com/blog/visual-guide-lumbar-osteophytes-bone-spurs
[/bg_collapse]