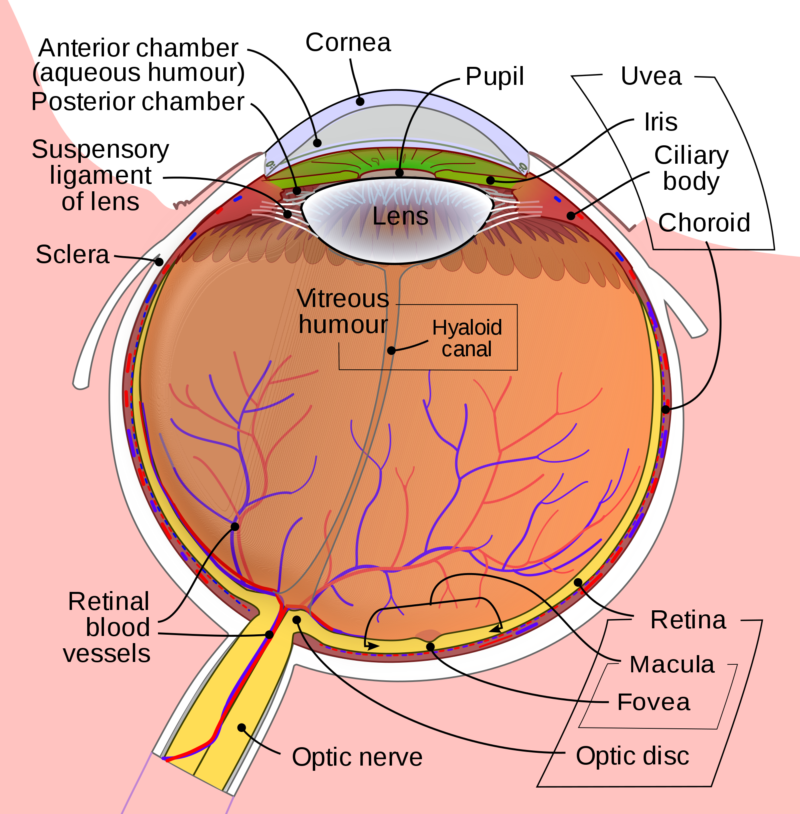
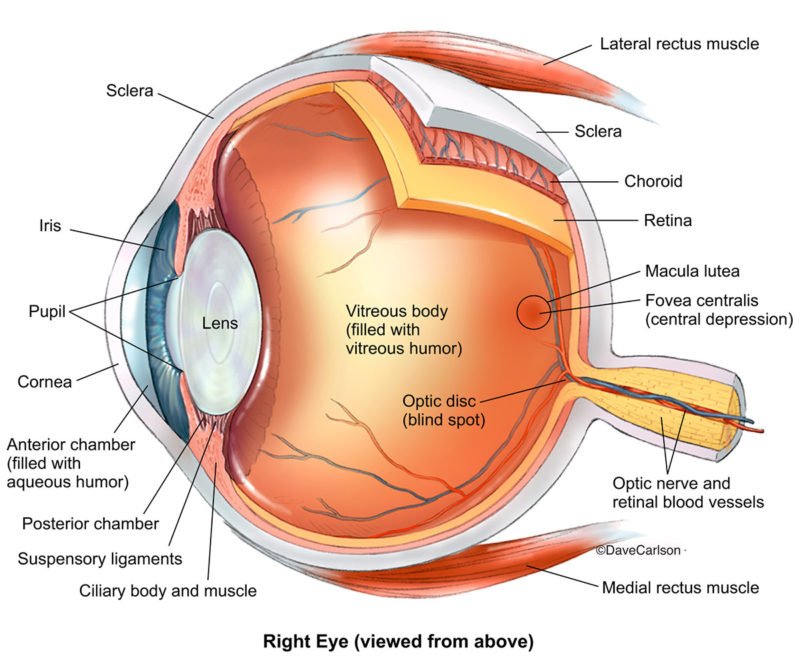
Detach Retina/Retinal detachment (RD), defined as the separation of the neurosensory retina from the underlying retinal pigment epithelium (RPE), can cause devastating visual loss. With advances in surgical techniques, the anatomical reattachment rate has greatly increased, especially after repeated surgery [rx, rx]. However, the final visual outcome remains, in many cases, disappointing once the retinal detachment involving the macula. Even with total retinal reattachment, long-term post-operative VA may lie anywhere in the range of 0.2 to 0.4 [rx]. Photoreceptor apoptosis has been postulated to be the main reason for such visual loss [rx–rx], alongside other structural changes in the retina such as glial scarring [rx]. Neuroprotection has thus become a focus of research to achieve a better visual outcome by preventing or reducing photoreceptor cell death.
Retinal detachment is a disorder of the eye in which the retina separates from the layer underneath.[rx] Symptoms include an increase in the number of floaters, flashes of light, and worsening of the outer part of the visual field.[rx][rx] This may be described as a curtain over part of the field of vision.[rx] In about 7% of cases, both eyes are affected.[rx] Without treatment, permanent loss of vision may occur.[rx]
Types of Detach Retina
Retinal detachment (RD) is broadly classified into three types based on clinical appearance and underlying etiology.
- Rhegmatogenous retinal detachment (RRD) – where the RD develops due to a retinal break (‘rhegma’, meaning rent or a fissure) [rx]. Fluid, from the vitreous cavity, passes through the retinal break into the potential space under the retina, leading to separation of the retina from the underlying choroid. This requires surgical treatment.
- Tractional retinal detachment (TRD) – which occurs due to pre-retinal membrane formation and scarring that pulls the retina from its attachment. This may require surgery depending on the extent of the RD. The commonest causes of TRD are diabetes, Eales’s disease, sickle cell retinopathy, and trauma.
- Exudative and serous retinal detachments – occur due to abnormalities in water transport across the bed of the retina (retinal pigment epithelium) or in its blood supply.
Tractional and exudative/serous retinal detachments are less common and will not be discussed in this paper.
Causes of Detach Retina
Rhegmatogenous
Caused by breaks in the retina, Associated with
- Age
- Myopia
- Cataract surgery
- Trauma
- Degenerative retinal lesions
- Stickler’s syndrome
- Juvenile X-linked retinoschisis
- Marfan’s syndrome
Tractional
Caused by chronic traction from scars on the retinal surface and across the vitreous cavity. Associated with
- Proliferative diabetic retinopathy
- Proliferative vitreoretinopathy
- Retinopathy of prematurity
- Penetrating eye injury
- Sickle cell retinopathy
- Retinal vein occlusion
Exudative
It happens when fluid collects under your retina, but there’s no tear. It can affect both eyes. This type of detachment often comes from an eye injury or as a complication of a wide range of diseases. They include various inflammatory and kidney diseases, as well as Lyme disease, eye tumors, and severe high blood pressure.
Caused by leakage of fluid into the subretinal space. Associated conditions
- Inflammatory (uveitis, scleritis)
- Hydrostatic (malignant hypertension, toxemia of pregnancy)
- Neoplastic (choroidal melanoma, haemangioma, metastasis)
- Vascular (Coat’s disease, retinal macroaneurysm)
- Maculopathy (neovascular macular degeneration, central serous chorioretinopathy)
- Congenital disorders (nanophthalmos, optic disc pit)
- Post cataract surgery (aphakia/pseudophakia) especially if the posterior capsule is ruptured during surgery and/or there is a vitreous loss.
- Yag laser capsulotomy.
- Lattice degeneration of the retina.
- Symptomatic (flashes/floaters) retinal tears.
- Ocular trauma
- RD in one eye
- Family history of RD
- Certain genetic disorders such as Marfan’s syndrome, Stickler’s syndrome.
- Pre-existing retinal diseases like coloboma choroid, retinoschisis.
- Following acute retinal infections as in acute retinal necrosis syndrome (ARN) or CMV retinitis.
- Glaucoma
- AIDS[rx]
- Cataract surgery[rx]
- Diabetic retinopathy[rx][rx]
- Eclampsia[rx]
- Family history of retinal detachment[rx]
- Homocysteinuria[rx]
- Malignant hypertension[rx]
- Metastatic cancer, which spreads to the eye (eye cancer)[rx]
- Retinoblastoma[rx]
- Severe myopia[rx]
- Smoking and passive smoking[rx]
- Stickler syndrome[rx]
- Von Hippel-Lindau disease[rx]
Symptoms of Detach Retina
A rhegmatogenous retinal detachment is commonly preceded by a posterior vitreous detachment which gives rise to these symptoms
- The detachment is visible as a grey, mobile membrane inside the eye.
- Intraocular pressure may be reduced
- The red reflex is usually pale, or grey, rather than the normal orange
- When examining the eye using a slit lamp, you may see pigment cells in the vitreous.
- Very brief flashes of light (photopsia) in the extreme peripheral (outside of center) part of a vision
- A sudden dramatic increase in the number of floaters
- A ring of floaters or hairs just to the temporal (skull) side of the central vision
Although most posterior vitreous detachments do not progress to retinal detachments, those that do produce the following symptoms
- The sudden appearance of many floaters — tiny specks that seem to drift through your field of vision
- Flashes of light in one or both eyes (photopsia)
- Blurred vision
- Gradually reduced side (peripheral) vision
- A curtain-like shadow over your visual field
- The dense shadow that starts in the peripheral vision and slowly progresses towards the central vision
- The impression that a veil or curtain was drawn over the field of vision
- Straight lines (scale, the edge of the wall, road, etc.) that suddenly appear curved (positive Amsler grid test)
- Central visual loss.
In the event of an appearance of sudden flashes of light or floaters, an eye doctor needs to be consulted immediately.[rx] Any loss of vision is also a medical emergency.
Diagnosis of Detach Retina
- A retinal examination – The doctor may use an instrument with a bright light and special lenses to examine the back of your eye, including the retina. This type of device provides a highly detailed view of your whole eye, allowing the doctor to see any retinal holes, tears or detachments.
- Retinal detachment can be examined – by fundus photography or ophthalmoscopy. Fundus photography generally needs a considerably larger instrument than the ophthalmoscopy but has the advantage of availing the image to be examined by a specialist at another location and/or time, as well as providing photo documentation for future reference.
- Modern fundus photographs – generally recreate considerably larger areas of the fundus than what can be seen at any one time with handheld ophthalmoscopes.
- Ultrasound – has diagnostic accuracy similar to that of examination by an ophthalmologist.[rx] The recent meta-analysis shows the diagnostic accuracy of emergency department (ED) ocular ultrasonography is high. The sensitivity and specificity ranged from 97% to 100% and 83% to 100%.[rx]
- The typical feature of retinal detachment – when viewed on ultrasound, is “flying angel sign”. It shows the detached retina moving with a fixed point under the B mode, linear probe 10 MHz.[rx]
Treatment of Detach Retina
There are several methods of treating a detached retina, each of which depends on finding and closing the breaks that have formed in the retina. All three of the procedures follow the same three general principles:
- Find all retinal breaks
- Seal all retinal breaks
- Relieve present (and future) vitreoretinal traction
- Laser coagulation – the laser light enters the eye via the pupil. The laser energy is absorbed in the retinal pigment epithelium, leading to heat (ca. 60 °C) and coagulation necrosis [rx, rx]. Cryocoagulation involves freezing of the eyeball all the way from the outside to the retina by application of a cryoprobe (ca. –80 °C). Both procedures are followed after a few days by the formation of a scar, but only if the retina is in contact with the underlying retinal pigment epithelium. Therefore, scar induction by either laser coagulation or cryocoagulation is effective only for prevention of detachment in a still-attached retina; both forms of coagulation are pointless if detachment has already occurred.
- Funduscopy – A detachment is recognized by the dune-like appearance and mobility of the retina, and the hole responsible for the detachment can often be discerned. The procedures employed for surgical management of retinal detachment are scleral buckling and vitrectomy. Here too laser coagulation or cryocoagulation is used for hole closure, but only after surgery to repair the detachment. Data for both of these surgical options are available from recent prospective randomized clinical trials.
- Scleral buckling – After precise localization of all retinal breaks and marking of the sclera, the holes are treated with cryopexy for scar induction. The traction exerted on the holes by the vitreous body is then reduced by a foam sponge sutured to the sclera [rx]
- Scleral buckle surgery – is an established treatment in which the eye surgeon sews one or more silicone bands (or tires) to the sclera (the white outer coat of the eyeball). The bands push the wall of the eye inward against the retinal hole, closing the break or reducing fluid flow through it and reducing the effect of vitreous traction thereby allowing the retina to re-attach. Cryotherapy (freezing) is applied around retinal breaks prior to placing the buckle. Often subretinal fluid is drained as part of the buckling procedure
- Pneumatic retinopexy – This operation is generally performed in the doctor’s office under local anesthesia. It is another method of repairing a retinal detachment in which a gas bubble (SF6[rx] or C3F8[rx] gas) is injected into the eye after which laser or freezing treatment is applied to the retinal hole. The patient’s head is then positioned so that the bubble rests against the retinal hole. Patients may have to keep their heads tilted for several days to keep the gas bubble in contact with the retinal hole. The surface tension of the gas/water interface seals the hole in the retina, and allows the retinal pigment epithelium to pump the subretinal space dry and “suck the retina back into place”.
- Vitrectomy – Vitrectomy begins with the removal of the vitreous humor causing the retinal detachment, followed by displacement of the subretinal fluid by means of a heavy tamponade (perfluorodecalin or perfluorocarbon) and scarring of the retina by laser coagulation or cryocoagulation. The vitreous is then replaced by a tamponade[rx], which holds the retina against the underlying retinal pigment epithelium until a firm scar has formed around the retinal hole. A mixture of air and gas or a silicone oil tamponade can be chosen for this purpose. The air/gas mixture is usually chosen in simpler situations (e.g., when the hole is at the top of the eyeball). The advantage of the air/gas tamponade is that it is absorbed and thus does not require removal.
- Injecting air or gas into your eye – In this procedure, called pneumatic retinopexy, the surgeon injects a bubble of air or gas into the center part of the eye (the vitreous cavity). If positioned properly, the bubble pushes the area of the retina containing the hole or holes against the wall of the eye, stopping the flow of fluid into space behind the retina. Your doctor also uses cryopexy during the procedure to repair the retinal break.
- Indenting the surface of your eye – This procedure, called scleral (SKLAIR-ul) buckling, involves the surgeon sewing (suturing) a piece of silicone material to the white of your eye (sclera) over the affected area. This procedure indents the wall of the eye and relieves some of the force caused by the vitreous tugging on the retina. If you have several tears or holes or an extensive detachment, your surgeon may create a scleral buckle that encircles your entire eye like a belt. The buckle is placed in a way that doesn’t block your vision, and it usually remains in place permanently.
- Draining and replacing the fluid in the eye – In this procedure, called vitrectomy, the surgeon removes the vitreous along with any tissue that is tugging on the retina. Air, gas or silicone oil is then injected into the vitreous space to help flatten the retina.
Health Tips for Home Treatment
Retinal detachment may cause you to lose vision. Depending on your degree of vision loss, your lifestyle might change significantly.
You may find the following ideas useful as you learn to live with impaired vision:
- Get glasses – Optimize the vision you have with glasses that are specifically tailored for your eyes. Request safety lenses to protect your better-seeing eye.
- Brighten your home – Have proper light in your home for reading and other activities.
- Make your home safer – Eliminate throw rugs and place colored tape on the edges of steps. Consider installing motion-activated lights.
- Enlist the help of others – Tell friends and family members about your vision problems so they can help you.
- Get help from technology – Digital talking books and computer screen readers can help with reading, and another new technology continues to advance.
- Check into transportation – Investigate vans and shuttles, volunteer driving networks, or ride shares available in your area for people with impaired vision.
- Talk to others with impaired vision – Take advantage of online networks, support groups, and resources for people with impaired vision.
References
[bg_collapse view=”button-orange” color=”#4a4949″ expand_text=”Show More” collapse_text=”Show Less” ]
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3275330/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1705859/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2405853/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3948016/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5525625/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6253314/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5638983/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3536954/
- https://en.wikipedia.org/wiki/Retinal_detachment
- https://nei.nih.gov/health/retinaldetach/retinaldetach
- https://www.medicalnewstoday.com/articles/170635.php
- https://www.webmd.com/eye-health/types-retinal-detachment
- https://www.medicinenet.com/retinal_detachment/article.htm
- https://medlineplus.gov/retinaldetachment.html
- https://www.aao.org/eye-health/diseases/detached-torn-retina-symptoms
- https://www.mayoclinic.org/detached-retina-retinal-detachment/
[/bg_collapse]

Visitor Rating: 5 Stars