Corneal transplantation is one of the most prevalent and successful forms of solid tissue transplantation. Despite favorable outcomes, immune-mediated graft rejection still remains the major cause of corneal allograft failure. While ‘low risk’ graft recipients with uninflamed graft beds enjoy a success rate of approximately 90%, the rejection rates in inflamed graft beds or ‘high risk’ recipients often exceed 50% despite maximal immune suppression. In this review we discuss the critical facets of corneal alloimmunity, including immune and angiogenic privilege, mechanisms of allosensitization, cellular and molecular mediators of graft rejection, and allotolerance induction.
Corneal transplantation, also known as corneal grafting, is a surgical procedure where a damaged or diseased cornea is replaced by donated corneal tissue (the graft). When the entire cornea is replaced it is known as penetrating keratoplasty and when only part of the cornea is replaced it is known as lamellar keratoplasty. Keratoplasty simply means surgery to the cornea. The graft is taken from a recently dead individual with no known diseases or other factors that may affect the chance of survival of the donated tissue or the health of the recipient.
Anatomy of Corneal Transplantation
Macroanatomy
- The cornea is a transparent avascular structure that protects structures inside the eye and contributes to two-thirds of its refractive power. The cornea is convex, has a diameter of approximately 11.5 mm, and increases in thickness from the center (550-565 μm) to the periphery (610-640 μm).[rx] The cornea is densely innervated by long ciliary nerves that originate in the ophthalmic division of the trigeminal nerve.
Microanatomy
- The layers anteroposteriorly include the epithelium, Bowman’s layer, stroma, Descemet’s membrane, and endothelium.[rx]
- The epithelium is the main barrier to the eye, provides a smooth optical surface and performs immunological functions. It consists of 5 to 7 cell layers in the center and 7 to 10 cell layers in the periphery, with an approximate thickness of 50 μm. The limbal stem cell hypothesis suggests the proliferation of stem cells and transient amplifying cells in the periphery with central migration to replace cells lost on the surface.[rx]
- Bowman’s layer is a tough tissue composed of primarily type I and V collagen and is an acellular condensate of the stroma. It contributes to the corneal shape.
- The corneal stroma provides mechanical strength and refractive power and consists of regularly arranged collagen fibers, glycosaminoglycans, and interconnected keratocytes, in packed layers or lamellae. At the corneal center, there are 200 lamellae, with a much higher packing density and interconnectivity in the anterior area compared to the posterior.
- In DSEK/DSAEK, when the air bubble is introduced to separate the endothelium and DM part of the posterior stroma adheres to the DM, suggesting a natural cleavage plane in the stroma ten μm above the DM.[rx]There have been suggestions that this area of the posterior stroma is anatomically distinct and has been named pre-Descemet’s layer or Dua’s layer.[rx]
- DM is a 7-10 micrometer structure that consists of Type IV collagen and laminin and is secreted by endothelial cells continuously.[rx] The corneal endothelium is a simple cuboidal monolayer of cells that are rich in mitochondria and are responsible for maintaining transparency.
Types of Corneal Transplantation
- Full Thickness Corneal Transplant – If the doctor does a penetrating keratoplasty (PK), all the layers of your cornea get replaced. The surgeon sews the new cornea onto your eye with stitches thinner than hair. You might need this procedure if you have a severe cornea injury or bad bulging and scarring. It has the longest healing time.
- Partial Thickness Corneal Transplant- During deep anterior lamellar keratoplasty (DALK), the surgeon injects air to lift off and separate the thin outside and thick middle layers of your cornea, then removes and replaces only those. People with keratoconus or a corneal scar that hasn’t affected the lower layers may have this done. The quality requirements of the donated cornea aren’t as strict, and the healing time is shorter than a full thickness transplant. Because your eye itself isn’t opened up, it’s unlikely the lens and iris could be damaged, and there’s less chance of an infection inside your eye.
- Endothelial Keratoplasty – About half of the people who need cornea transplants each year have a problem with the innermost layer of the cornea, the endothelium.
- Penetrating Keratoplasty (PK) – this is a full-thickness corneal transplant used to treat diseases that affect the full thickness of the cornea.
- Endothelial Keratoplasty (DSAEK, DMEK) – this is a partial-thickness corneal transplant used to treat diseases where only the endothelium (the back layer of the cornea) is affected, such as Fuchs Endothelial Dystrophy.
- Anterior Lamellar Keratoplasty (ALK, DALK) – this is a partial thickness corneal transplant used to treat diseases which affect the stroma (the front layers of the cornea), such as Keratoconus or certain dystrophies.
Indications of Corneal Transplantation
Indications include the following
- Optical – To improve visual acuity by replacing the opaque or distorted host tissue by clear healthy donor tissue. The most common indication in this category is pseudophakic bullous keratopathy, followed by keratoconus, corneal degeneration, keratoglobus and dystrophy, as well as scarring due to keratitis and trauma.
- Tectonic/reconstructive – To preserve corneal anatomy and integrity in patients with stromal thinning and descemetoceles, or to reconstruct the anatomy of the eye, e.g. after corneal perforation.
- Therapeutic – To remove inflamed corneal tissue unresponsive to treatment by antibiotics or anti-virals.
- Cosmetic – To improve the appearance of patients with corneal scars that have given a whitish or opaque hue to the cornea.
- Penetrating keratoplasty – indications include keratoconus, ectasias, corneas degenerations, dystrophies, keratitis, congenital opacities, chemical/mechanical corneal trauma, and re-grafts.
- The reported leading indications – in a region are dependent on sociopolitical, geographical and economic factors and may not accurately reflect the most common aetiologies of corneal pathology.[rx]
- Endothelial keratoplasty (EK) – includes PLK, DLEK, DSEK, DSAEK, DMEK, and DMAEK. EK procedures are not appropriate for patients with healthy corneal endothelium such as keratoconus.
- EK indications include – Fuch’s endothelial dystrophy, posterior polymorphous dystrophy, congenital hereditary endothelial dystrophy, bullous keratopathy, iridocorneal endothelial syndrome, and failed EKs.
- Deep anterior lamellar keratoplasty (DALK) – indications include those that relate to the pathology of the anterior cornea (epithelium, Bowman’s layer, and stroma), such as keratoconus and corneal scars.
- Keratoconus – to learn about why a corneal transplant is required for keratoconus,
- Corneal clouding – there are many conditions that may cause the cornea to become swollen and cloudy, such as Fuchs’ endothelial dystrophy and pseudophakic bullous keratopathy. In severe cases the cornea may develop small blisters on the surface which can be very painful.
- Corneal infection – Infections of the cornea may be bacterial, fungal, or viral. Severe corneal infections may cause scarring, thinning, or perforation of the cornea. Herpes simplex is the most common viral infection that may lead to scarring.
- Corneal dystrophy – some hereditary conditions called dystrophies cause the cornea to become opaque or irregular and may require corneal transplantation.
- Corneal injury – injuries to the cornea, such as penetrating eye injuries, may cause corneal scarring that affects the vision and requires corneal transplantation.
The Diagnoses That Indicate I Could Need a Cornea Transplant
Conditions that damage your corneas and impair your ability to see clearly may require a corneal transplant. These conditions include:
- Fuchs’ dystrophy – a condition in which the inner layer (endothelial) cells of the cornea die, causing the cornea to swell and thicken and vision to become blurred
- Keratoconus – a condition that causes the cornea to be cone-shaped instead of dome-shaped
- Infections – which cause permanent damage to the cornea
- Traumatic injuries – that penetrate or scar the cornea
- Previous eye surgeries – that damaged the cornea
- Bullous keratopathy – a blister-like swelling of the cornea that causes eye discomfort, pain, and blurred vision
- Keratitis – an inflammation of the cornea caused by viruses, bacteria, fungi, or parasites
Contraindications of Corneal Transplantation
- There are absolute and relative contraindications for corneal transplantation in each country that are highly region-dependant. The National Health Services (NHS) Blood and Transplant Agency in the United Kingdom (UK) has the following absolute contraindications transplant unlikely to restore corneal function or integrity or remove tissue that would otherwise have led to further damage to the eye.
Before The Procedure
- Once you and your eye doctor decide a cornea transplant is the best option for you, your name is placed on a list at a local eye bank. You may need to wait a few days to weeks for suitable tissue from a donor eye to become available for a corneal transplant.
- Before a donor cornea is released for use in transplant surgery, it is checked for clarity and screened for the presence of any diseases such as hepatitis and AIDS, in accordance with the Eye Bank Association of America’s strict medical standards and FDA regulations.
- Only corneas that meet these stringent guidelines are used in corneal transplant surgery to ensure the health and safety of the graft recipient.
During The Cornea Transplant
- Your eye surgeon will first administer either local or general anesthesia, depending on your health, age, eye injury or disease, and whether or not you prefer to be asleep during the procedure.
- If local anesthesia is used, an injection is made into the skin around your eye to relax the muscles that control blinking and eye movements, and eye drops are used to numb your eye. You will be awake during the procedure and most people don’t report any discomfort.
- After the anesthesia has taken effect, an instrument called a lid speculum is used to keep your eyelids open. Your surgeon then measures the affected corneal area to determine the size of the donor tissue needed.
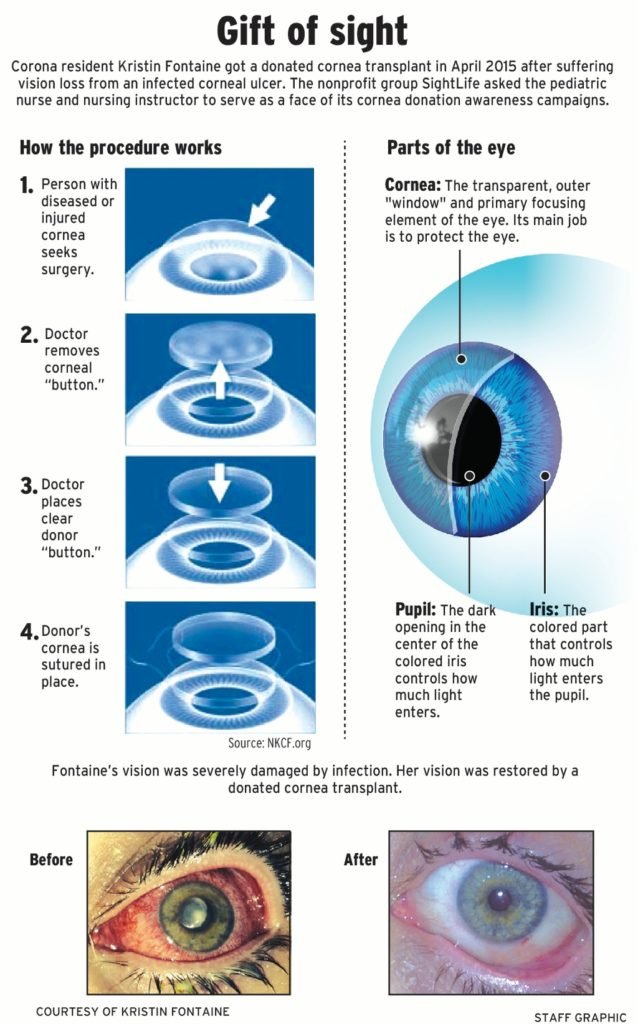
Traditional corneal transplant surgery – During traditional corneal transplant surgery, or penetrating keratoplasty (PK), a circular button-shaped, full-thickness section of tissue is removed from the diseased or injured cornea using either a surgical cutting instrument called a trephine or a femtosecond laser
- A matching “button” from the donor tissue is then positioned and sutured into place. The sutures (stitches) remain in place typically for a year or more after surgery. Lastly, a plastic shield is placed over your eye to protect it during healing.
- Penetrating keratoplasty surgery generally takes one to two hours and most procedures are performed on an outpatient basis, meaning you can go home a short while after the surgery (though you will need someone to drive you home).
Endothelial keratoplasty. In the past decade, a newer version of corneal transplant surgery called endothelial keratoplasty (EK) has been introduced for certain corneal conditions.
- Endothelial keratoplasty selectively replaces only the innermost layer of the cornea (endothelium) and leaves the overlying healthy corneal tissue intact. The endothelium controls the fluid balance in the cornea, and if it becomes damaged or diseased, this can cause significant corneal swelling and loss of vision.
- In EK, the surgeon makes a tiny incision and places a thin disc of donor tissue containing a healthy endothelial cell layer on the back surface of your cornea. An air bubble is used to position the new endothelial layer into place. The small incision is self-sealing and typically no sutures are required.
Recovering From A Cornea Transplant
Total cornea transplant recovery time can be up to a year or longer. Initially, your vision will be blurry for the first few months — and in some cases may be worse than it was before — while your eye gets used to its new cornea.
- As your vision improves – you gradually will be able to return to your normal daily activities. For the first several weeks, heavy exercise and lifting are prohibited. However, you should be able to return to work within a week after surgery, depending on your job and how quickly your vision improves.
- Steroid eye drops – will be prescribed for several months to help your body accept the new corneal graft, as well as other medications to help control infection, discomfort, and swelling. You should keep your eye protected at all times by wearing a shield or a pair of eyeglasses so that nothing inadvertently bumps or enters your eye.
- If stitches – were used in your surgery, they usually are removed three to 17 months post-surgery, depending on the health of your eye and the rate of healing. Adjustments can be made to the sutures surrounding the new corneal tissue to help reduce the amount of astigmatism resulting from an irregular eye surface.
- As with any type of surgery – always follow the instructions of your eye surgeon to help minimize corneal transplant complications and expedite healing.
Treatment of Corneal Transplantation
Corticosteroids
- Corticosteroids represent the key medication for the management of corneal transplantation. They can be used pre-, intra-, or postoperatively. Systemic corticosteroids have been used, either as monotherapy or in combination with other immunosuppressive agents to prevent corneal graft rejection in HR settings as well as to treat acute rejection.
Cyclosporine A
- Cyclosporine A (CsA) is a macrolide with powerful immunosuppressive activity that modulates T cell function.[rx] It is an 11-amino acid peptide isolated from the fungus Tolypocladium inflatum. Cyclosporine A acts by binding to the intracellular protein cyclophilin, which inhibits the activity of calcineurin enzyme, blocking nuclear factor activation.[rx]
- Cyclosporine A inhibits the interleukin (IL)-2 pathway, leading to a decrease in the synthesis and secretion of several pro-inflammatory cytokines such as IL-2, IL-4, interferon-γ (IFN- γ), tumor necrosis factor-α (TNF- α), and thus results in inhibition of helper and cytotoxic T cell differentiation.
Tacrolimus
- Tacrolimus, or FK506, is a macrolide antibiotic with potent immunosuppressive activity, which is isolated from the soil fungus Streptomyces Tsukubaensis. This calcineurin inhibitor has a mode of action similar to that of CsA. Its mechanism of action initiates with binding to a class of peptidyl-prolyl cis-trans isomerases, known as FK506-binding proteins (FKBPs), especially FKBP-12.[rx,rx]
Mycophenolate Mofetil
- Mycophenolate mofetil (MMF) is another type of immunosuppressant used systemically after organ transplantation.[104] It is the pro-drug of the active substance mycophenolic acid (MPA), a potent inhibitor of inosine monophosphate dehydrogenase, which inhibits the de novo synthesis of guanosine nucleotides, resulting in selective inhibition of T- and B-lymphocyte proliferation.[rx,rx]
- Mycophenolate mofetil has been demonstrated to be effective and safe in kidney and heart transplantations at a dose of 3 g per day and for liver transplantation using a dose of 2 g per day.[rx,rx,rx,rx] The most common reported side effects are infections, anemia, leukopenia, and gastrointestinal disturbances; however, blood monitoring is generally unnecessary and reserved for special situations, such as severe adverse events or treatment fail
Rapamycin (Sirolimus, Rapamune)
- Rapamycin is a bacterial macrolide isolated from Streptomyces hygroscopicus, which has antifungal and immunosuppressive properties.[rx] Rapamycin forms a complex with the immunophilin FK binding-protein (FKBP-12), and the rapamycin-FKBP-complex inhibits the mammalian target of rapamycin (mTOR).[rx]
- Despite having a structure similar to that of tacrolimus, rapamycin is not a calcineurin inhibitor and thus not nephrotoxic. It acts by decreasing IL-2-mediated activation of T-lymphocytes with a blood concentration range of 12-20 ng/mL.[rx,rx]
Complication
Organ rejection is when the body’s immune system sees transplanted tissue as something that shouldn’t be there and tries to get rid of it. Rejection is a problem for up to 3 out of 10 people who have a corneal transplant.
Warning signs of your body trying to reject your cornea transplant include:
- Eye pain
- Being extra sensitive to light
- Redness of the eye
- Cloudy or hazy vision
- Infection – in the cornea or inside the eye
- Bleeding
- Glaucoma (increased pressure inside your eye)
- Fluid leakage from your cornea
- Detached retina (tissue lining the back of the eye pulls away from the eye)
- Visual acuity problems (sharpness of the vision) caused by an irregular curve in the shape of the cornea
- Detachment of the corneal transplant (for the endothelial transplant which is held in place by an air bubble)
- detached retina (where the tissue lining the back of the eye pulls away from the eye)
- glaucoma (through increased pressure inside the eye)
- Even when corneal transplants work as they should, other eye problems could limit the quality of your vision. For instance, the new cornea might not be curved regularly (called astigmatism). Or you could have an eye disease such as macular degeneration, glaucoma, or diabetic retinopathy.
- Cornea scarring because of an injury or an infection
- Corneal ulcers or “sores” from an infection
- A medical condition that makes your cornea bulge out (keratoconus)
- Thinning, clouding, or swelling of the cornea
- Inherited eye diseases, such as Fuchs’ dystrophy and others
- Problems caused by an earlier eye operation
References
[bg_collapse view=”button-orange” color=”#4a4949″ expand_text=”Show More” collapse_text=”Show Less” ]
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5492649/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3081421/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3872837/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2810523/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4874505/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4155896/
- https://www.statpearls.com/kb/viewarticle/19997/
- https://www.ncbi.nlm.nih.gov/books/NBK470340/
- https://www.ncbi.nlm.nih.gov/books/NBK519043/
- https://jamanetwork.com/journals/jamaophthalmology/fullarticle/2474372
- https://www.springer.com/gp/book/9783319240503
- https://en.wikipedia.org/wiki/Corneal_transplantation
- https://www.allaboutvision.com/conditions/cornea-transplant.htm
- https://www.aao.org/eye-health/treatments/what-to-expect-when-you-have-corneal-transplant
- https://www.webmd.com/eye-health/cornea-transplant-surgery
- https://www.lei.org.au/services/eye-health-information/corneal-transplants/
- https://www.nkcf.org/corneal-transplants/
- https://my.clevelandclinic.org/health/treatments/17714-cornea-transplant/recovery-and-outlook
- https://www.nhs.uk/conditions/cornea-transplant/
[/bg_collapse]